1.4 Health Disparities
Sections:
1.4.1 Health Disparities Defined
Health disparities exist in all age groups, including older adults. Even though life expectancy and overall health have improved in recent years for most Americans, not all older adults benefit equally because of factors such as economic status, race, and gender (CDC, 2017).
According to the 2018 United States (U.S.) Census report, the year 2030 marks a demographic turning point for the United States. The nation’s population is projected to age considerably and become more racially and ethnically diverse. The population of people who are more than one race is projected to be the fastest-growing racial or ethnic group over the next several decades, followed by Asian Americans and Hispanic/Latino Americans (CDC, 2022d).
1.4.2 Vulnerable Populations
“Vulnerable populations include patients who are elderly, racial or ethnic minorities, elderly, socioeconomically disadvantaged, uninsured, or those with certain medical conditions. Members of vulnerable populations often have health conditions exacerbated by unnecessarily inadequate healthcare” (Waisel, 2013).
I. The Elderly
According to the U.S. Census Bureau (2018), although declining fertility plays a role, the baby boomers are the driving force behind America’s aging. As one of the largest generations in the country, boomers leave a substantial imprint on the population. They swelled the ranks of the young when they were born and then the workforce as they entered adulthood. Now, boomers will expand the number of older adults as they age. Starting in 2030, when all boomers will be older than 65, older Americans will make up 21% of the population, up from 15% today. By 2060, nearly one in four Americans will be 65 years and older, the number of 85-plus will triple, and the country will add a half million centenarians (Fig. 1-3). For the older population, the biggest increase is expected in the decade from 2020 to 2030, when the population aged 65 and over is projected to increase by 18 million, from 56 million to 74 million (U.S. Census Bureau, 2018).
Figure 1-4
A Growing Population of Older Adults
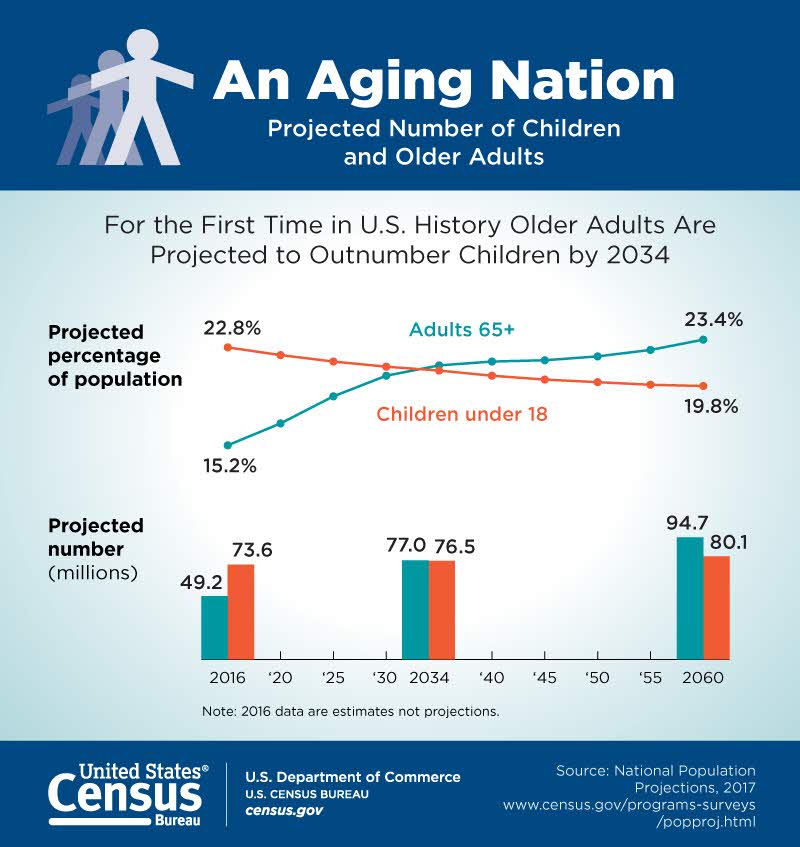
(U.S. Census Bureau, 2018)
With this swelling number of older adults, the country could see greater demands for healthcare, in-home caregiving, and assisted living facilities. In addition to the direct relationship between age and the prevalence of chronic conditions, nearly 82% of Medicare beneficiaries have at least one chronic condition, and 64% have multiple conditions (Anderson & Horvath, 2002; Wolff, 2002). Treating these conditions may require daily medications, specialized equipment, or care coordination (U.S. Department of Health and Human Services, 2010b).
II. Race and Ethnicity
Though health indicators such as life expectancy and infant mortality have improved for most Americans, some people from racial and ethnic minority groups experience a disproportionate burden of preventable disease, death, and disability compared with non-Hispanic White people (CDC, 2022d).
Despite decades of effort, disparities persist, and changes in the racial and ethnic composition of the population have important consequences for the nation’s health (CDC, 2020). Moreover, these disparities sometimes persist even when accounting for other demographic and socioeconomic factors, like age or income. For example, according to the U.S. Government Accountability Office (2021):
- Between March 2020 and June 2021, Hispanic or Latino and non-Hispanic Black people were hospitalized with COVID-19 at a rate 2.8 times higher than non-Hispanic White people when taking age into account.
- From 2011–2016, Black women living in rural counties experienced 59.3 deaths per 100,000 live births, compared to 19.7 for White women in the same counties, according to CDC data.
- In 2018, the diabetes age-adjusted mortality rate was higher among Black people (49.7 deaths per 100,000 people) and American Indian/Alaska Native people (40.0 deaths) than White people (24.8 deaths).
- Black veterans with cancer and cardiovascular-related illnesses had lower survival rates than White veterans.
III. Socioeconomic Status
The interconnectedness of health and socioeconomic status cannot be overstated. A person’s income and other measures of social status affect health directly and indirectly by impeding access to care (Barr, 2019; Khullar & Chokshi, 2018). Individuals with low socioeconomic status have greater rates of behavioral risk factors such as substance use, smoking, insufficient physical activity, and obesity (Khullar & Chokshi, 2018). People with lower socioeconomic status also experience worse care than higher-income individuals (AHRQ, 2022; Khullar & Chokshi, 2018; Ndugga & Artiga, 2021). Disparities exist in access to health insurance, general access to healthcare, and timely access to services (AHRQ, 2022). Approximately 9% of the population is uninsured (Khullar & Chokshi, 2018), creating barriers to routine preventative healthcare and challenges in coordinating care, which may result in increased visits to the emergency department by this population.
In the U.S., income-based health disparities are among the largest in the world, where adults living in poverty are five times as likely to report being in fair or poor health (Khullar & Chokshi, 2018). Poverty affects approximately 43 million Americans and is associated with an increased risk of diseases and premature death (Office of Disease Prevention and Health Promotion [ODPHP], n.d.). The distribution of wealth in the U.S. is even more unequal than income, which plays a crucial role in intergenerational health disparities (Khullar & Chokshi, 2018). During the last two decades, the income of poor and middle Americans has decreased (Thorpe et al., 2017). The widening income gap and the percentage of children experiencing poverty are crucial socioeconomic status challenges that impact health.
Inequitable access to resources and opportunities can be caused by a variety of reasons, leading to poverty (ODPHP, n.d.). For example, according to Givens et al. (2020), counties that were among the least healthy had greater rates of poverty, uninsured people, and unemployment than the rest of the country (Fig. 1-4):
Figure 1-5
Gaps in Health Factors in the Year 2020
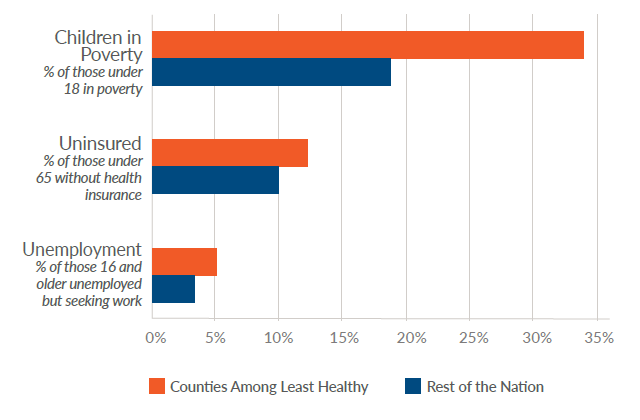
(Givens et al., 2020)
Review the full report (Givens et al., 2020): 2020 County Health Rankings Key Findings Report
IV. The Uninsured
In the U.S., access to healthcare is often synonymous with having health insurance (Kirby et al., 2022). Although the rate of uninsured Americans decreased under the Affordable Care Act (Uberoi et al., 2016), there has been a recent rise in the uninsured rate again (Morenz, 2021). This increase began prior to the COVID-19 pandemic, although the virus did not help matters. From 2017 to 2019, the uninsured rate rose by 1.7%, most likely due to various policy changes to the Patient Protection and Affordable Care Act (ACA) and Medicaid (Finegold et al., 2021). Since 2016, there has been a disturbing increasing trend in uninsured children in the U.S. The number of children who lacked consistent private or public insurance coverage increased between 2016 and 2019 (Yu et al., 2021). According to Finegold et al. (2021), when compared to other Americans, the uninsured are disproportionately likely to be African American or Latino, be young adults, have low incomes, and/or live in states that have not expanded Medicaid. Some of the other variations were due to states which decided not to expand their Medicaid under the ACA (Larson et al., 2020). Some of it is due to the variation in the availability of employer-sponsored coverage (particularly for low-wage workers) from state to state (Dworsky et al., 2022).
In 2019, 14.5% of adults aged 18–64 were uninsured. Among uninsured adults aged 18–64, the most common reasons for being currently uninsured were they perceived that they could not afford the cost of coverage, followed by not being eligible, not wanting coverage, the process of signing up was too difficult or confusing, they could not find a plan that meets their needs, or they signed up for coverage but the plan has not started yet. In 2019, the percentage of adults who were uninsured due to cost was higher among women, adults aged 50–64, and adults in fair or poor health. The percentage of adults who were uninsured due to ineligibility did not vary by age but was higher among women and adults in fair or poor health. In contrast, the percentage of adults who were uninsured because coverage was not needed or wanted was higher among men, adults aged 18–29, and adults with excellent, very good, or good health (Cha & Cohen, 2020). Individuals without health insurance experience barriers to health care, such as not having a usual source of care and postponing or forgoing care due to cost, which may lead to negative health outcomes (Freeman et al., 2008; Tolbert et al., 2022).
Review the full data brief (Cha & Cohen, 2020): Reasons for Being Uninsured Among Adults Aged 18–64 in the United States, 2019
1.4.3 Social Determinants of Health
Social determinants of health (SDOH) is a relatively new term in healthcare. Social determinants of health (SDOH) have a major impact on people’s health, well-being, and quality of life. Unfortunately, SDOH also contribute to wide health disparities and inequities. For example, people who don’t have access to grocery stores with healthy foods are less likely to have good nutrition which raises their risk of health conditions like heart disease, diabetes, and obesity. This situation even lowers life expectancy relative to people with access to healthy foods. Just promoting healthy choices won’t eliminate these and other health disparities. Instead, public health organizations and their partners in sectors like education, transportation, and housing must take action to improve the conditions in people’s environments (U.S. Department of Health and Human Services [DHHS], n.d.)
Healthy People 2030
In 1979, the Surgeon General issued a landmark report titled “Healthy People: The Surgeon General’s Report on Health Promotion and Disease Prevention” (ODPHP, 2021). A year later, in 1980, the Office of Disease Prevention and Health Promotion (ODPHP) released Healthy People 1990, which was followed in later decades by new iterations of the Healthy People initiative, each building on the last. This initiative provides 10-year, measurable public health objectives and tools to help track progress toward achieving them (ODPHP, 2021). Healthy People 2030, launched in August 2020, is the fifth and most current iteration of the Healthy People initiative. It builds on knowledge gained over the last 4 decades and has an increased focus on health equity, social determinants of health, and health literacy with a new focus on well-being (ODPHP, 2021).
Five Key Areas of Social Determinants of Health
SDOH are one of three priority areas for Healthy People 2030, along with health equity (i.e., the attainment of the highest level of health for all people) and health literacy (i.e., the ability to navigate, understand, and use health information and services). Healthy People 2030 sets data-driven national objectives in the five key areas of SDOH (Fig. 1-5): economic stability, education access and quality, healthcare access and quality, neighborhood and built environment, and social and community context (CDC, 2022e).
Figure 1-6
Five Key Areas of Social Determinants of Health

(CDC, 2022e)
I. Economic Stability
In the U.S., 1 in 10 people live in poverty, and many cannot afford healthy foods, healthcare, and housing (Semega et al., 2019). Healthy People 2030 focuses on helping more people achieve economic stability. People with steady employment are less likely to live in poverty and more likely to be healthy, but many people have trouble finding and retaining a job. People with disabilities, injuries, or conditions like arthritis may be especially limited in their ability to work. In addition, many people with steady work still do not earn enough to afford the things they need to stay healthy. Employment programs, career counseling, and high-quality childcare opportunities can help more people find and retain jobs. In addition, policies to help people pay for food, housing, healthcare, and education can reduce poverty and improve health and well-being. The goal of this key area is to help people earn steady incomes that allow them to meet their health needs (DHHS, n.d.).
II. Education Access and Quality
People with higher levels of education are more likely to be healthier and live longer. Healthy People 2030 focuses on providing high-quality educational opportunities for children and adolescents and helping them do well in school. Children from low-income families, children with disabilities, and children who routinely experience forms of social discrimination — like bullying — are more likely to struggle with math and reading. They are also less likely to graduate from high school or attend college. As a result, they are less likely to get safe, high-paying jobs and more likely to have health problems like heart disease, diabetes, and depression. In addition, some children live in places with poorly performing schools, and many families cannot afford to send their children to college. The stress of living in poverty can also affect children’s brain development, making it harder for them to do well in school. Interventions to help children and adolescents do well in school and help families pay for college can have long-term health benefits. The goal of this key area is to increase educational opportunities and help children and adolescents do well in school (DHHS, n.d.).
III. Healthcare Access and Quality
Many people in the U.S. don’t get the healthcare services they need (CDC, 2021b). Healthy People 2030 focuses on improving health by helping people get timely, high-quality healthcare services. About 1 in 10 people in the U.S. don’t have health insurance (Berchick et al., 2018). People without insurance are less likely to have a primary care provider, and they may be unable to afford the healthcare services and medications they need. Strategies to increase insurance coverage rates are critical for making sure more people get important healthcare services, like preventive care and treatment for chronic illnesses. Sometimes people don’t get recommended healthcare services, like cancer screenings, because they don’t have a primary care provider. Other times, it’s because they live too far away from healthcare providers who offer them. Interventions to increase access to healthcare professionals and improve communication — in person or remotely — can help more people get the care they need. The goal of this key area is to increase access to comprehensive, high-quality healthcare services (DHHS, n.d.).
IV. Neighborhood and Built Environment
The neighborhoods people live in have a major impact on their health and well-being (CDC, 2018). Healthy People 2030 focuses on improving health and safety in the places where people live, work, learn, and play. Many people in the U.S. live in neighborhoods with high rates of violence, unsafe air or water, and other health and safety risks. Racial/ethnic minorities and low-income people are more likely to live in places with these risks. In addition, some people are exposed to things at work that can harm their health, like secondhand smoke or loud noises. Interventions and policy changes at the local, state, and federal levels can help reduce these health and safety risks and promote health. For example, providing opportunities for people to walk and bike in their communities — like by adding sidewalks and bike lanes — can increase safety and help improve health and quality of life. The goal of this key area is to create neighborhoods and environments that promote health and safety (DHHS, n.d.).
V. Social and Community Context
People’s relationships and interactions with family, friends, co-workers, and community members can have a major impact on their health and well-being. Healthy People 2030 focuses on helping people get the social support they need in the places where they live, work, learn, and play. Many people face challenges and dangers they can’t control — like unsafe neighborhoods, discrimination, or trouble affording the things they need. These challenges can have a negative impact on health and safety throughout life. Positive relationships at home, work, and in the community can help reduce these negative impacts. But some people — like children whose parents are in jail and adolescents who are bullied — often don’t get support from loved ones or others. Interventions to help people get the social and community support they need are critical for improving health and well-being. The goal of this key area is to increase social and community support (DHHS, n.d.).

