2.2 Outpatient Care
Outpatient services occur in a facility or setting where there is no need for an overnight stay. The types of procedures and tests offered might include wellness and prevention services, such as annual exams; diagnostic services, such as lab tests and imaging scans; treatment, such as day surgeries or chemotherapy; and rehabilitation, such as physical therapy or addiction treatment. Because no overnight stay is involved, outpatient services usually cost less (George et al., 2021). Some facilities specialize in one kind of treatment or procedure, such as an orthopedic surgery center, although many can be provided in one place. Three types of outpatient care include primary care, ambulatory surgical care, and urgent care.
2.2.1 Primary Care
I. Description
Primary care is the entry point into the healthcare system and is one of the most utilized outpatient services. Primary care clinics are the point of delivery of individual care based on care over time and are not disease-oriented but focus on preventive and sick visits. Primary care providers see patients who do not require immediate medical care for life-threatening conditions.
Primary care services cover a range of prevention, wellness, and treatment for common illnesses. Primary care providers include doctors, nurses, nurse practitioners, and physician assistants. They often maintain long-term relationships with you and advise and treat you on a range of health-related issues. They may also coordinate your care with specialists.
The four pillars of primary care, represented in Figure 2-1, are (Starfield, 1998):
- A patient’s first contact with the healthcare system
- Continuity of care over time
- Comprehensiveness (i.e., concern for the whole patient rather than a disease or part of the patient)
- Coordination of care
Figure 2-1
The Four Pillars of Primary Care
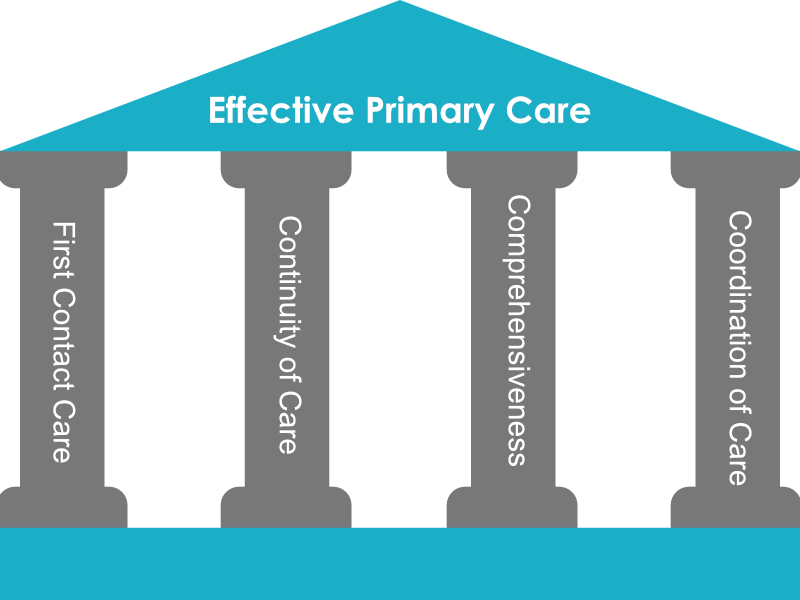
(Starfield, 1998)
II. Venues
There are several venues for the delivery of primary care. A major one is the private clinic of physicians. Another primary care venue is the public or non-profit community health center, which provides access to primary care for low-income, uninsured, and minority populations (Bodenheimer & Pham, 2010). Other government settings include clinics for the military (such as those run by the Veterans Health Administration), prisons, the Indian Health Service, and centers for migrants and the homeless (Bodenheimer & Pham, 2010). Urban public and teaching hospitals may also have outpatient clinics for primary care services, typically serving underserved populations (Bodenheimer & Pham, 2010). In addition, many integrated care systems, such as Kaiser Permanente and Geisinger Health System, provide primary care as part of their integrated systems, which cover primary, specialty, emergency, and hospital care (Bodenheimer & Pham, 2010). Finally, workplace wellness programs and retail clinics provide some primary care services by providing screening, health promotion, and basic prevention services (Baicker et al., 2010; RAND Corporation, 2010).
Retail clinics located in pharmacies, general stores, and department stores, have emerged as alternative sites for primary care (Hoff & Prout, 2019). These clinics are operated mainly by pharmacy chains, such as CVS Health and Walgreens, and department stores, such as Target and Walmart, where the clinics are also located, but hospitals and large healthcare systems are also beginning to offer healthcare at such sites (Hoff & Prout, 2019). Companies known more for their technology services, like Amazon and Apple, are either planning to enter the retail clinic market or have already done so. A positive feature of retail clinics is that they have walk-in availability, extended hours compared to physicians’ offices, and convenient access points (Hoff & Prout, 2019). They tend to be staffed by non-physician practitioners, such as NPs or PAs. Retail clinics treat a limited number of conditions and needs, such as skin conditions, sore throats, pregnancy testing, infections, diabetes screening, and immunizations (Hoff & Prout, 2019).
The following two models of care are being employed to increase efficiencies in primary care delivery: patient-centered medical homes and accountable care organizations.
- Patient-centered medical homes (PCMHs) have several characteristics that should positively impact the delivery of primary care: (1) each patient has an ongoing relationship with a primary care provider; (2) the primary care provider directs the medical team; (3) the primary care provider has responsibility for caring for all the patient’s health needs through all stages of the patient’s life; (4) patient care is coordinated across all healthcare settings; (5) services are safe, evidence-based and of high quality, with patients actively participating in decision-making; (6) patients have access to care; (7) payment systems recognize the added value of PCMHs (Rittenhouse et al., 2011). The Affordable Care Act has promoted PCMHs by paying state Medicaid programs to shift patients into medical homes, funding new PCMH models of care, and supporting the information technology needed for care coordination in PCMHs (Hoff et al., 2012).
- Accountable care organizations (ACOs) are groups of providers in an area including primary and specialty care physicians, hospitals, and others who coordinate and integrate their care for patients (Centers for Medicare & Medicaid Services [CMS], 2023). ACOs aim to ensure patients receive the proper care at the right time without duplication of services and medical errors. ACOs differ from PCMHs in that payment is tied to the performance of the ACO, thus conferring financial risk for members. In contrast, PCMHs have no direct relationship between payment and membership. When an ACO succeeds in both efficiency and high quality, it will share in the savings. ACOs were initiated by the Patient Protection and Affordable Care Act (ACA). They were first implemented in the Medicare shared savings program, but the ACA also supports pilot programs to extend the model to private payers and Medicaid.
2.2.2 Ambulatory Surgery Centers
Improvements in surgical equipment, techniques, and anesthesia have led to more and more surgeries being performed on an outpatient basis in the United States. Compared to inpatient surgery, outpatient surgery has the advantage of convenient hours and locations, a lower risk of infection, and recovery from surgery at home (Plotzke & Courtemanche, 2011). The disadvantage is that reduced professional oversight during the recovery period can lead to complications. Ambulatory surgery can be performed in either hospital same-day surgery departments or free-standing ambulatory surgical centers (Munnich & Parente, 2014). In 2014, 66% of all surgeries were in the outpatient (i.e., ambulatory) setting (Rechtoris, 2017). This number increased significantly from 1981, when outpatient surgeries were only 19% of all surgeries (Munnich & Parente, 2014). Common surgeries and procedures performed in the ambulatory setting include those for back problems, cataracts, cancers, colonoscopy, diverticula, inguinal hernia repair, gallstones, and many orthopedic problems (Cullen et al., 2009). Surgeries not done on an outpatient basis are those with high risk, long duration, or serious physical or mental limitations for the patient during recovery. An example is open-heart surgery.
More serious surgeries are being performed on an outpatient basis as improvements in drugs and techniques reduce the surgical time, the invasiveness of the procedure, and the length of the recovery period. Knee replacement is an example of a complex surgery that used to take several hours to perform, was extremely invasive, and required a long, supervised physical recovery period, but that is now primarily an outpatient procedure (Meissner, 2015). Even hip replacements are performed on an outpatient basis (Cluett, 2023).
Compared to hospital-based surgical centers, ambulatory surgical centers (ASCs) are perceived to be more conveniently located and to have better scheduling for both physician and patient, greater physician and patient satisfaction, similar quality, and lower costs (Munnich & Parente, 2014; Plotzke & Courtemanche, 2011). For example, there is some evidence that ASCs have lower costs and similar health outcomes, such as mortality rates (Chukmaitov et al., 2008; Hollenbeck et al., 2015; Munnich & Parente, 2014). Disadvantages of ASCs include physician self-referral patterns and a concern that ASCs serve the less sick, more profitable patients, leaving the sicker, less profitable patients in hospital-based centers (Hollenbeck et al., 2010; Koenig & Gu, 2013; Plotzke & Courtemanche, 2011).
2.2.3 Urgent Care
Outpatient clinics and urgent care facilities often serve as alternative places to receive healthcare when individuals cannot get to a hospital. During a public health emergency, these settings may see an increase in the number of patients they treat.
Urgent care is provided outside the emergency department setting in urgent care centers (UCCs) that provide care on a walk-in basis, have extended hours into the evening Monday to Friday and at least one day over the weekend, and have on-site laboratories and radiology (American College of Emergency Physicians [AECP], 2017; Le & Hsia, 2016). The scope of services in these centers is broader than those in many primary care offices or retail clinics and falls somewhere between that of a primary care practitioner’s office and an emergency department (ACEP, 2017; Le & Hsia, 2016). Services focus on acute episodic care including care for minor illnesses and emergencies such as upper respiratory infections, urinary tract infections, backaches, sprains, strains, lacerations, burns, and minor fractures (Corwin et al., 2016; Stoimenoff & Dunn, 2018). Medical care is typically performed by primary care physicians, APRNs, and PAs (ACEP, 2017; Le & Hsia, 2016). UCCs have expanded rapidly over the past few years with around 400–500 new centers opening each year (Stoimenoff & Dunn, 2018). This expansion has been in response to difficulties in seeing primary care practitioners on an urgent basis and after hours, high emergency department costs, and long emergency department waiting times (Stoimenoff & Dunn, 2018; Villasenor & Krouse, 2016). The ability to get same-day test results and medications also makes them popular. Some individuals (around 30–40% of UCC admissions) use UCCs because they do not have a regular source of primary care (Stoimenoff & Dunn, 2018). Studies have shown that areas with more urgent care alternatives to emergency departments have lower emergency department use for low acuity diagnoses (Llovera et al., 2019).
Knowledge Check
Match each statement to the correct center to complete the sentences.

