4.1 Basic Concepts
4.1.1 Population Health Management
Populations refer to individuals and the context where people live, work and play in local communities (Carlson, 2020). The term population health is described as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group” (Kindig & Stoddart, 2003).
Population health (PopH) is extremely broad and “recognizes the range of social, economic, and physical environmental factors that contribute to health” (Public Health Agency of Canada, 2012). Focusing on a population’s health versus targeting individual health has become an essential framework for delivering healthcare. The American Hospital Association (2023), a major health sector stakeholder, defines Population Health Management (PHM) by adding and integrating a strong management component. The new PHM pathway has transitioned from a disease-only treatment model for individuals to a population health strategy focused on groups, and, finally to a management model that requires clinical effectiveness, cost-effectiveness, and safer health outcomes.
In 1979, a landmark document titled “Healthy People: The Surgeon General’s Report on Health Promotion and Disease Prevention” recommended for the first time a coordinated national healthcare strategy (Office of Disease Prevention and Health Promotion [ODPHP], 2021). Then, in 1980, ODPHP released Healthy People 1990, which was followed in later decades by new iterations of the Healthy People initiative, each building on the last. At the end of every decade, the U.S. Department of Health and Human Services assesses progress toward achieving Healthy People’s 10-year national objectives. Over the years, the five editions of Healthy People have regularly provided evidence for setting health goals and objectives to address the enormous variation in the distribution of disease and morbidity for various at-risk and minority populations (ODPHP, n.d.). The latest version of our national public health objectives, Healthy People (HP) 2030, lists 355 core objectives ranging from reducing chronic diseases to mitigating the contagious disease that reached a pandemic stage, COVID-19. This expansive document not only provides evidence-supported objectives but also identifies metrics to help track them. The following HP 2030 goals serve as guidelines for all collaborative health efforts, including PHM (Centers for Disease Control and Prevention [CDC], 2020).
- Attain healthy, thriving lives and well-being free of preventable disease, disability, injury, and premature death.
- Eliminate health disparities, achieve health equity, and attain health literacy to improve the health and well-being of all.
- Create social, physical, and economic environments that promote the full potential for health and well-being for all.
- Promote healthy development, healthy behaviors, and well-being across all life stages.
- Engage leadership, key constituents, and the public across multiple sectors to act and design policies that improve the health and well-being of all.
4.1.2 The Triple Aim
Health policy experts responded to the challenge of improving health and produced several major national health commentaries to guide new models. Two prominent reports that attracted enormous attention and concern were the Institute of Medicine’s “To Err is Human” and “Crossing the Quality Chasm: A New Health System for the 21st Century” (National Academy of Medicine, 2000, 2001). All Americans should expect safe care, free from mistakes, and quality care that is accessible and effective. Both documents described crises within the health sector needing drastic and immediate change. However, a seminal article introduced one of the most important PHM components – the Triple Aim. The Triple Aim concept was a proposed solution to an existing model first introduced in William Kissick’s book, Medicine’s Dilemmas: Infinite Needs Versus Finite Resources in 1994. This first model, known as The Iron Triangle (Fig. 4-1), focused on three key aims of healthcare delivery: access, quality, and cost (Berwick et al., 2008).
Figure 4-1
Three Key Aims of the Iron Triangle
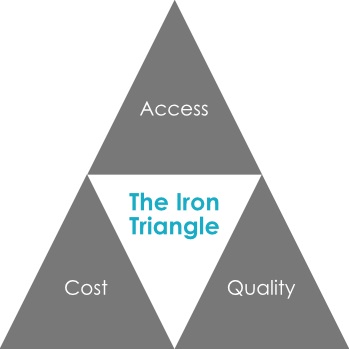
(Berwick et al., 2008)
The Triple Aim of Healthcare was presented by the Institute for Healthcare Improvement in 2007 (Berwick et al., 2008). It was defined as an attempt to realign the three aims of healthcare previously identified in the Iron Triangle. The Institute for Healthcare Improvement (IHI) intended for this new model to change the dynamics of healthcare from one focused on an individual to one encompassing population and society at large. It also wanted to shift our thinking from a healthcare system utilized to cure each illness that arises for individuals on a case-by-case basis to one that encompasses the maintenance of the health and wellness of populations. This new model would include treating chronic conditions (i.e., those that develop over time and are ongoing) rather than acute conditions (i.e., those that develop suddenly and are limited in duration). The IHI realized that treating chronic diseases such as diabetes, heart disease, cancer, and others cost the U.S. healthcare system billions of dollars. Today, it costs us over a trillion dollars (Waters & Graf, 2018). Costs and patient outcomes were the driving forces in the IHI’s development of the Triple Aim. The Triple Aim has the following three pillars (Berwick et al., 2008):
- Improving the patient experience of care
- Improving the health of populations
- Reducing the per capita cost of healthcare
Improving individual patient experience had previously been understood as the main focus of improvement for healthcare delivery; however, the Triple Aim also included the elements of population health and cost (Fig. 4-2). As a result, these are now considered critical elements in determining the improvements made in the healthcare industry.
Figure 4-2
The Three Key Elements of the Triple Aim
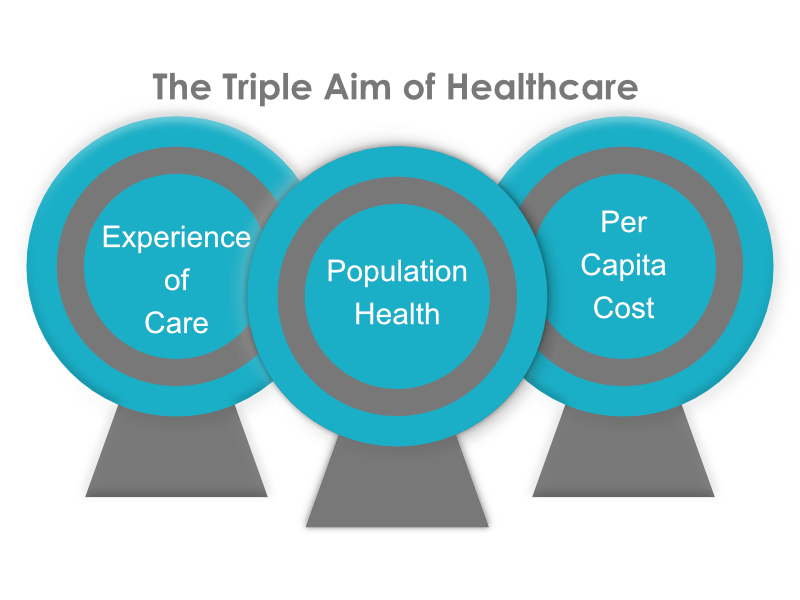
(Berwick et al., 2008)

