18 Obstetrics
Learning Objectives
- Identify the processes involved in human reproduction and childbirth
- Evaluate the specialty of obstetrics
- Differentiate the medical terms used in obstetrics and use correct abbreviations
- Recognize the medical specialties associated with obstetrics
- Discover common complications and procedures related to obstetrics
Obstetrics Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize related to obstetrics.
Introduction to Obstetrics
Obstetrics is a specialty that is concerned with the mother and fetus during pregnancy, childbirth, and the immediate postpartum period. Obstetricians study obstetrics and gynecology and are referred to as OB/GYN, Obstetrics and Gynecology.
Watch this video:
Media 18.1. Reproductive System, Part 4 – Pregnancy & Development: Crash Course A&P #43 [Online video]. Copyright 2015 by CrashCourse.
Practice Medical Terms Related to Obstetrics
Fertilization
Fertilization occurs when sperm and an oocyte combine. Because each of these reproductive cells is a haploid cell containing half of the genetic material needed to form a human being, their combination forms a diploid cell. This new single cell is called a zygote.
Most of the time, a woman releases a single egg during an ovulation cycle.
- In approximately 1% pof ovulation cycles, two eggs are released and both are fertilized.
- Two zygotes form, implant, and develop, resulting in the birth of dizygotic (or fraternal) twins. Because dizygotic twins develop from two eggs fertilized by two sperm, they are no more identical than siblings born at different times.
- Less common, one zygote can divide into two separate offspring during early development. This results in the birth of monozygotic (or identical) twins.
A full-term pregnancy lasts approximately 270 days (approximately 38.5 weeks) from conception to birth. Because it is easier to remember the first day of the last menstrual period (LMP) than to estimate the date of conception, obstetricians set the due date as 284 days (approximately 40.5 weeks) from the LMP. This assumes that conception occurred on day 14 of the woman’s cycle, which is usually a good approximation. The 40 weeks of an average pregnancy are usually discussed in terms of three trimesters, each approximately 13 weeks. During the second and third trimesters, the pre-pregnancy uterus is about the size of a fist and grows dramatically to contain the fetus, causing a number of anatomical changes in the mother.
Stages of Childbirth
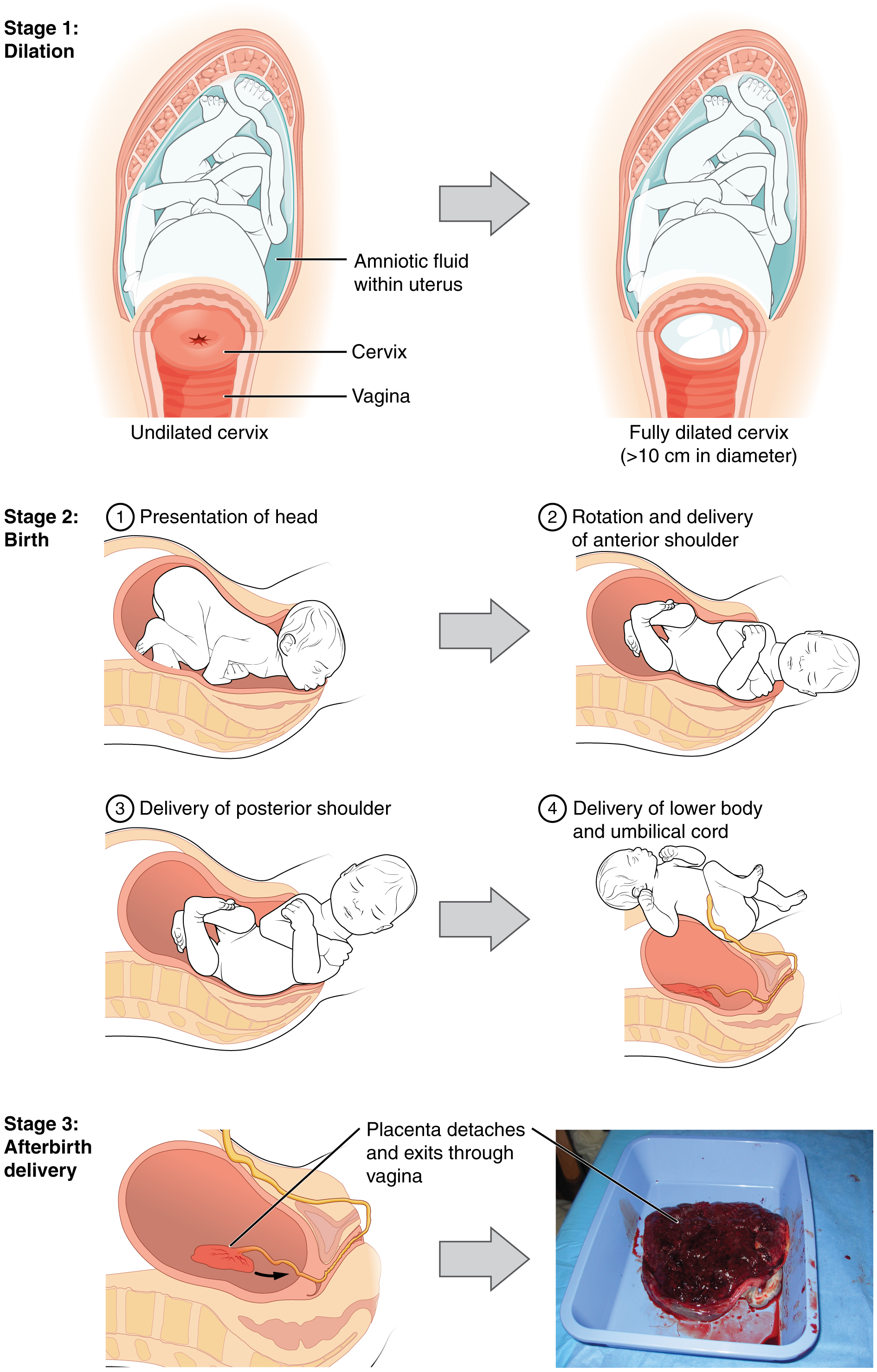
The process of childbirth can be divided into three stages (see Figure 18.1):
- cervical dilation
- expulsion of the newborn
- after birth
For vaginal birth to occur, the cervix must dilate fully to 10 cm in diameter, wide enough to deliver the newborn’s head. The dilation stage is the longest stage of labor and typically takes 6 to 12 hours. However, it varies widely and may take minutes, hours, or days, depending in part on whether the mother has given birth before. In each subsequent labor, this stage tends to be shorter.
Concept Check
- How is a due date determined?
- Explain the difference between a monozygotic pregnancy and a dizygotic pregnancy.
Homeostasis in the Newborn: Apgar Score
In the minutes following birth, a newborn must undergo dramatic systemic changes to be able to survive outside the womb. An obstetrician, midwife, or nurse can estimate how well a newborn is doing by obtaining an Apgar score. The Apgar score was introduced in 1952 by the anesthesiologist Dr. Virginia Apgar as a method to assess the effects on the newborn of anesthesia given to the laboring mother. Healthcare providers now use it to assess the general well-being of the newborn, whether or not analgesics or anesthetics were used.
The five criteria, skin color, heart rate, reflex, muscle tone, and respiration, are assessed and each criterion is assigned a score of 0, 1, or 2. Scores are taken one minute after birth and again five minutes after birth. Each time scores are taken, the five scores are added together. High scores (out of a possible 10) indicate the baby has made the transition from the womb well, whereas lower scores indicate that the baby may be in distress.
The technique for determining an Apgar score is quick and easy, painless for the newborn, and does not require any instruments except for a stethoscope. A convenient way to remember the five scoring criteria is to apply the mnemonic APGAR:
- Appearance (skin color)
- Pulse (heart rate)
- Grimace (reflex)
- Activity (muscle tone)
- Respiration
Of the five Apgar criteria, heart rate and respiration are the most critical. Poor scores for either of these measurements may indicate the need for immediate medical attention to resuscitate or stabilize the newborn. In general, any score lower than 7 at the 5-minute mark indicates that medical assistance may be needed. A total score below 5 indicates an emergency. Normally, a newborn will get an intermediate score of 1 for some of the Apgar criteria and will progress to a 2 by the five-minute assessment. Scores of 8 or above are normal.
Did you know?
Practice Terms Related to Obstetrics
Common Abbreviations for Obstetrics
Many terms and phrases related to obstetrics are abbreviated. Learn these common abbreviations by expanding the list below.
Medical Terms in Context
Diseases and Disorders Related to Obstetrics
Preeclampsia and Eclampsia
Preeclampsia and eclampsia refer to hypertensive disorders that occur during pregnancy among women without a history of high blood pressure. Signs and symptoms of preeclampsia include blood pressure at or greater than 140/90 mmHg at or after 20 weeks of pregnancy, edema, and protein in the urine. Women with preeclampsia are at risk of preterm birth. If the condition is severe enough to cause seizures or a coma, it is referred to as eclampsia. If not treated, preeclampsia and eclampsia can be fatal (Office of Communications, n.d.).
Ectopic Pregnancy
An ectopic pregnancy occurs when a fertilized egg implants outside of the uterus, usually in the fallopian tube. Risk factors include older age, smoking, the use of an intrauterine device, in vitro fertilization, and prior pelvic infections, including chlamydia. Signs and symptoms include pain in the abdomen or shoulder, vaginal bleeding, and dizziness. Treatment may involve surgery or the use of medication to stop the growth of ectopic tissue (Mummert & Gnugnoli, 2021; MedlinePlus, 2021a).
Miscarriage
Miscarriage, also known as spontaneous abortion, refers to the loss of pregnancy before the 20th week. It is the most common form of pregnancy loss. Risk factors include older maternal age, a history of miscarriages, disorders of the uterus or cervix, and chronic diseases such as polycystic ovary syndrome. Signs and symptoms include vaginal spotting, abdominal pain, and cramping. However, these symptoms can be confused with symptoms of an ectopic or normal pregnancy. Treatment is generally not required in women who miscarry early in their pregnancy. If tissue remains in the uterus after miscarriage, treatment includes the use of medication to aid expulsion or a surgical procedure called dilation and curettage (D&C) (Dugas & Slane, 2021; MedlinePlus, 2021b).
Medical Procedures Related to Obstetrics
In Vitro Fertilization (IVF)
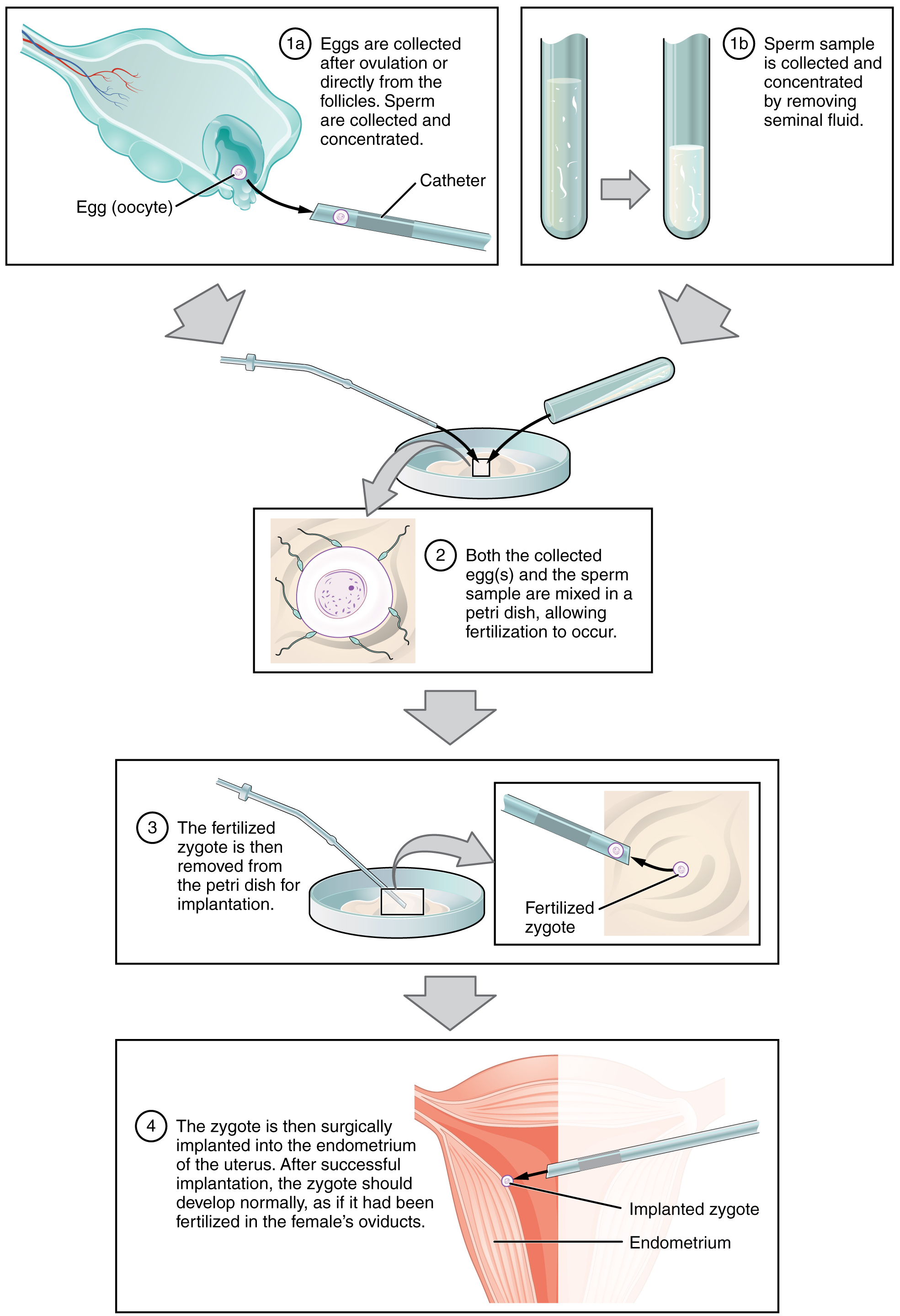
IVF, which stands for in vitro fertilization, is an assisted reproductive technology. In vitro, which in Latin translates to in glass, refers to a procedure that takes place outside of the body. There are many different indications for IVF. For example, a woman may produce normal eggs, but the eggs cannot reach the uterus because the uterine tubes are blocked or otherwise compromised. A man may have a low sperm count, low sperm motility, sperm with an unusually high percentage of morphological abnormalities, or sperm that are incapable of penetrating the zona pellucida of an egg. Figure 18.2 illustrates the steps involved in IVF.
Did you know?
According to the Centers for Disease Control and Prevention (n.d.-a), 6% of married women aged 15 to 44 years in the U.S. experience infertility.
Prenatal Screening and Diagnostic Testing
Obstetrics Vocabulary
Abortion
Intentional removal of a fetus from the uterus.
Alpha-fetoprotein test
Alpha-fetoprotein (AFP) is a protein that is produced during fetal development. The AFP test is an analysis of the mother’s blood serum to determine whether the level of AFP denotes a risk of a birth defect.
Amenorrhea
Absence of menstruation.
Amniocentesis
A procedure for obtaining amniotic fluid.
Amniotomy
Incision into the amnion to induce labor.
Apgar score
A technique used to assess the general wellbeing of a newborn. The newborn is assessed one minute after birth and again five minutes after birth.
Artificial insemination
A process where the semen is introduced into the vagina by mechanical means.
Breech
The position of the fetus is feet first. Ideally, the position of the fetus should be headfirst for a safer delivery.
Cesarean section
Delivery of the fetus through an abdominal incision.
Cephalopelvic disproportion
A condition where the infant’s head is larger than the mother’s pelvis.
Cerclage
A suture inserted into the cervix to prevent dilation and prevention miscarriage.
Chorioamnionitis
Inflammation of the chorion and amnion.
Choriocarcinoma
A malignant, fast-growing tumor that develops from trophoblastic cells (cells that help an embryo attach to the uterus and help form the placenta).
Chorionic villus sampling
A procedure in which tissue from the placenta is tested for fetal chromosomal disorders.
Colostrum
A thick, yellowish substance secreted from a mother’s breasts in the first postpartum days.
Dilation and curettage (D&C)
A procedure to scrape and remove tissue from the inner lining of the uterus. The cervix is dilated (made larger) and a curette (spoon-shaped instrument) is inserted into the uterus to remove tissue. The procedure is used to test tissue for signs of disease, after a miscarriage, or to treat certain conditions.
Dystocia
Slow or difficult labor.
Eclampsia
A very serious condition in pregnant women with hypertension; patients are at high risk of coma, convulsions, and even death.
Ectopic pregnancy
A pregnancy in which the fertilized ovum is implanted in any tissue other than the uterine wall.
Episiotomy
Incision made in the posterior vaginal wall and perineum that facilitates vaginal birth.
Fetal
Pertaining to the fetus.
Gestation
The period required for embryonic and fetal development in utero; pregnancy.
Gestational diabetes
Diabetes mellitus that occurs during pregnancy but resolves by the end of pregnancy in women without a history of diabetes.
Gestational hypertension
Elevated systolic and diastolic blood pressure in pregnant women.
Gravidity
The number of pregnancies, complete or incomplete, experienced by a woman.
Hyperemesis gravidarum
Excessive vomiting during pregnancy. Hyperemesis can occur with any pregnant woman, even a woman who miscarried. Often these women may require hospitalization for fluid and electrolyte intake.
Induction
The process of bringing on or starting labor through artificial means.
In vitro fertilization
A process where the ova is fertilized outside the body and then implanted into the uterus.
Lactic acid
A substance produced by the body, such as during strenuous exercise, that aids in various chemical processes in the body.
Meconium
Fetal wastes consisting of ingested amniotic fluid, cellular debris, mucus, and bile.
Microcephaly
A congenital abnormality where the head is small.
Midwifery
Practice of assisting in childbirth.
Natal
Pertaining to being born or birth.
Neonatal
Pertaining to the newborn’s first thirty days of life outside of the uterus.
Neonate
An infant during the first 28 days after birth.
Neonatologist
Physician who studies and treats disorders of the newborn.
Neonatology
A subspecialty of pediatric medicine concerned with the newborn.
Obstetrician
A doctor who specializes in caring for women during pregnancy and childbirth.
Obstetrics and gynecology
A branch of medicine that specializes in the care of women during pregnancy and childbirth and in the diagnosis and treatment of diseases of the female reproductive organs; also called OB/GYN.
Oligohydramnios
A condition of abnormally low amniotic fluid volume.
Oocyte
Immature egg cell.
Parturition
Childbirth.
Placenta abruptio
Occurs when the placenta prematurely becomes detached from the uterine wall, resulting in uterine bleeding, fetal distress, or fetal death; also known as abruptio placenta.
Placenta previa
Low placement of fetus within the uterus, which causes the placenta to partially or completely cover the opening of the cervix as it grows.
Polyhydramnios
A condition where there is excessive amniotic fluid in the placenta.
Postnatal
Pertaining to after birth.
Postpartum
The period of approximately 6 weeks immediately following childbirth.
Preeclampsia
The abnormal condition in pregnancy where the patient experiences hypertension, edema, and proteinuria.
Prenatal
Having to do with the time a female is pregnant, before birth occurs; also called antenatal.
Primigravida
First pregnancy.
Pseudocyesis
False pregnancy.
Puerperal
Pertaining to immediately after childbirth.
Puerperium
Time directly after childbirth (6 to 8 weeks after giving birth).
Sperm
Male gamete (spermatozoon).
Stillbirth
An infant who is born dead.
Teratogen
An agent capable of producing malformations in a developing embryo.
Teratology
A branch of embryology for the study of congenital malformations and developmental abnormalities.
Vaginal birth following a C-section
Delivery of an infant through the vagina in a female who has had a prior cesarean section.
Zygote
A single cell formed by the fusion of an egg and sperm; also called the fertilized egg.
Test Yourself
References
Centers for Disease Control and Prevention. (n.d.-a). Infertility FAQs. https://www.cdc.gov/reproductivehealth/infertility/index.htm
Centers for Disease Control and Prevention. (n.d.-b). Data & statistics on birth defects. https://www.cdc.gov/ncbddd/birthdefects/data.html
Centers for Disease Control and Prevention. (n.d.-c). Diagnosis of birth defects. https://www.cdc.gov/ncbddd/birthdefects/diagnosis.html
CrashCourse. (2019, November 23). Reproductive System, Part 4 – Pregnancy & Development: Crash Course A&P #43 [Video]. YouTube. https://youtu.be/BtsSbZ85yiQ
Dugas, C., & Slane, V. H. (2021). Miscarriage. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK532992/
MedlinePlus. (2021a). Ectopic pregnancy. U.S. National Library of Medicine. https://medlineplus.gov/ectopicpregnancy.html
MedlinePlus. (2021b). Miscarriage. U.S. National Library of Medicine. https://medlineplus.gov/miscarriage.html
Mummert, T., & Gnugnoli, D. M. (2021). Ectopic pregnancy. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK539860/
Office of Communications. (n.d.). About preeclampsia and eclampsia. Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health. https://www.nichd.nih.gov/health/topics/preeclampsia/conditioninfo
Image Descriptions
Figure 18.1 image description: This multi-part figure shows the different stages of childbirth. The top panel shows dilation of the cervix (undilated vs fully dilated), the middle panel shows birth (presentation of the head, rotation and delivery of anterior shoulder, delivery of posterior shoulder, delivery of lower body, and umbilical cord), and the bottom panel shows afterbirth delivery. [Return to Figure 18.1].
Figure 18.2 image description: This multi-part figure shows the different steps in in vitro fertilization. The top panel shows how the oocytes and the sperm are collected and prepared (text reads: 1a) eggs are collected after ovulation or directly from the follicles. Sperm is collected and concentrated. 1b) Sperm sample is collected and concentrated by removing seminal fluid). The next panel shows the sperm and oocytes being mixed in a petri dish (text labels read: 2) both the collected eggs and the sperm sample are mixed in a petri dish, allowing fertilization to occur). The panel below shows the fertilized zygote being prepared for implantation (text labels read: 3a) the fertilized zygote is then removed from the petri dish for implantation. 3b) fertilized zygote). The last panel shows the fertilized zygote being implanted into the uterus (text label reads: 4) The zygote is then surgically implanted into the endometrium of the uterus. After successful implantation, the zygote should develop normally, as if it had been fertilized in the female’s oviducts). [Return to Figure 18.2].
Male gamete (spermatozoon) (Betts et al., 2013)
Immature egg cell (Betts et al., 2013)
A single cell formed by the fusion of an egg and sperm; also called the fertilized egg (Betts et al., 2013)
Swelling due to excessive liquid in the tissues (Betts et al., 2013)
A process where the ova is fertilized outside the body and then implanted into the uterus (Betts et al., 2013)
A procedure in which tissue from the placenta is tested for fetal chromosomal disorders (Betts et al., 2013)
A procedure for obtaining amniotic fluid (National Library of Medicine, 2021)

