11 Lymphatic and Immune Systems
Learning Objectives
- Examine the anatomy of the lymphatic and immune systems
- Determine the main functions of lymphatic and immune systems
- Differentiate lymphatic and immune systems medical terms and common abbreviations
- Recognize the medical specialties associated with lymphatic and immune systems
- Discover common diseases, disorders, and procedures related to lymphatic and immune systems
Word Parts for the Lymphatic and Immune Systems
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Lymphatic and Immune Systems.
Introduction to the Lymphatic and Immune Systems
The lymphatic system is a series of vessels, ducts, and trunks that remove interstitial fluid from the tissues and return it to the blood. The lymphatic vessels are also used to transport dietary lipids and cells of the immune system. Cells of the immune system, lymphocytes, all come from the hematopoietic system of the bone marrow. Primary lymphoid organs, the bone marrow and thymus gland, are the locations where lymphocytes proliferate and mature. Secondary lymphoid organs are the site in which mature lymphocytes congregate to mount immune responses. Many immune system cells use the lymphatic and circulatory systems for transport throughout the body to search for and then protect against pathogens.
This chapter begins by describing the anatomy and physiology of the lymphatic system, whose immune functions lead us into a discussion of the body’s multifaceted defenses, which together make up the immune system. Since the lymphatic system shares organs with a number of other body systems, the pathology discussed near the end of this chapter mainly focuses on disorders of the immune system.
Watch this video:
Media 11.1 Lymphatic System: Crash Course A&P #44 [Online video]. Copyright 2015 by CrashCourse.
Practice Medical Terms Related to the Lymphatic and Immune Systems
Anatomy and Physiology of the Lymphatic and Immune Systems
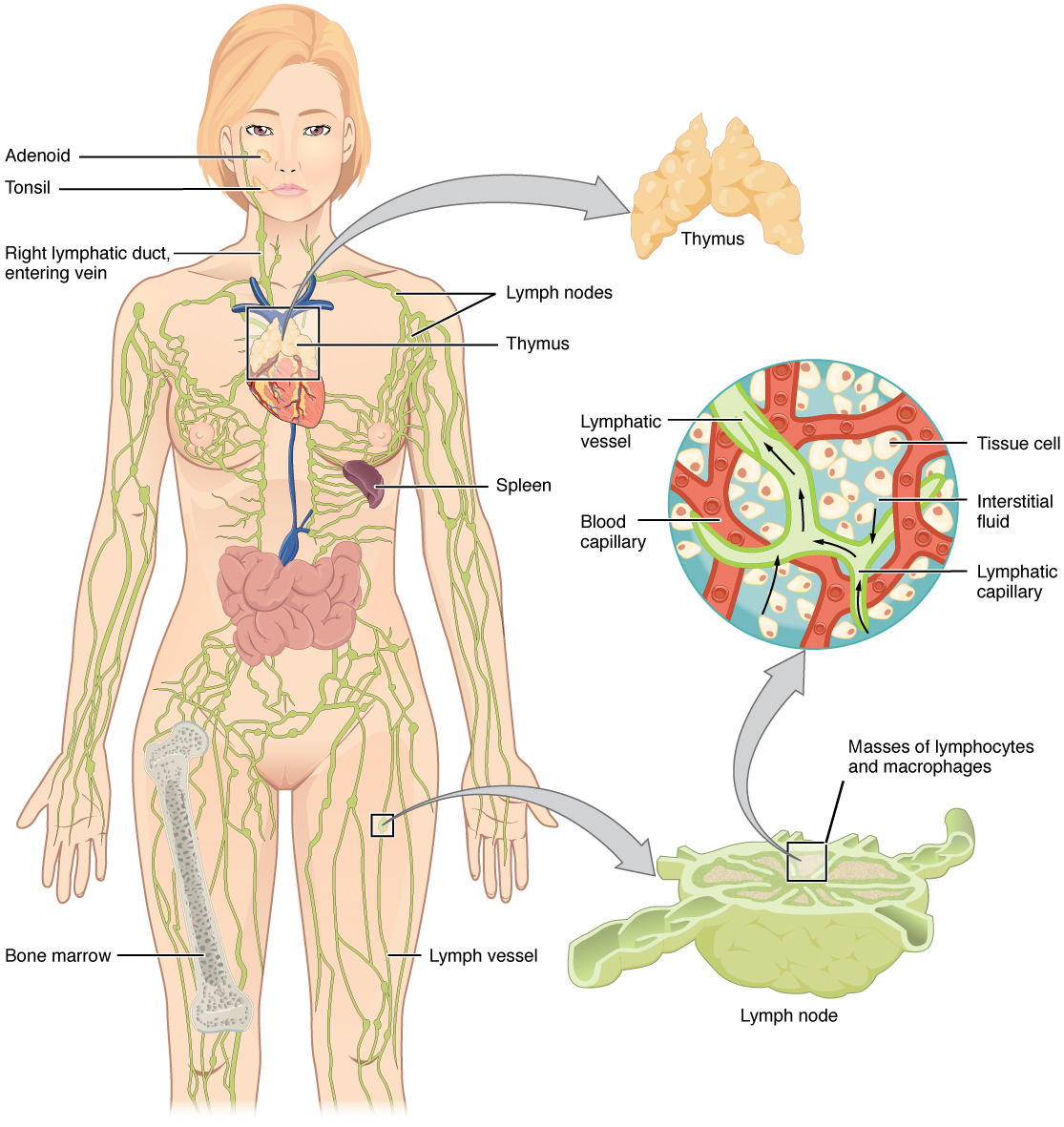
The lymphatic vessels begin as open-ended capillaries, which feed into larger and larger lymphatic vessels, and eventually empty into the bloodstream. Along the way, the lymph travels through the lymph nodes, which are commonly found near the groin, armpits, neck, chest, and abdomen. Humans have about 500 to 600 lymph nodes throughout the body (see Figure 11.1). Several organs and tissues that participate in immunity are also part of the lymphatic system.
Lymphatic Capillaries
An important function of the lymphatic system is to return the fluid (lymph) to the blood. Lymph may be thought of as recycled blood plasma. Blood pressure causes leakage of fluid from the blood capillaries, resulting in the accumulation of fluid in the interstitial space. In humans, 20 liters of plasma is released into the interstitial space of the tissues each day due to capillary leakage. The blood vessels reabsorb 17 liters of this interstitial fluid, leaving three liters in the tissues for the lymphatic system to transport back to the circulation. If the lymphatic system is damaged in some way, such as by being blocked by cancer cells or destroyed by injury, interstitial fluid accumulates in the tissue spaces, causing a condition called lymphedema.
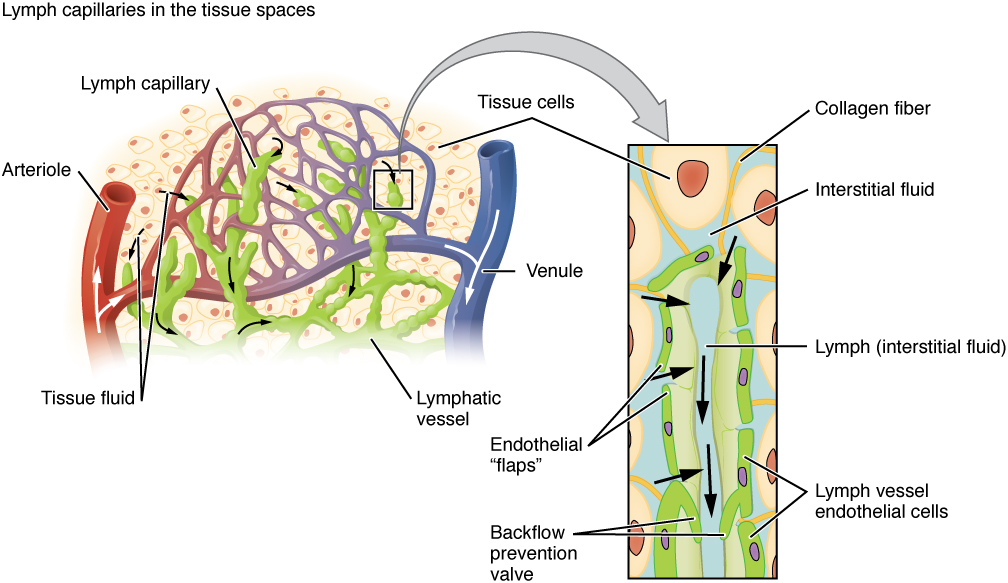
Lymphatic capillaries, also called the terminal lymphatics, are vessels where interstitial fluid enters the lymphatic system to become lymph. Located in almost every tissue in the body, these vessels are interlaced among the arterioles and venules of the circulatory system in the soft connective tissues of the body (see Figure 11.2). Exceptions are the central nervous system, bone marrow, bones, teeth, and the cornea of the eye, which do not contain lymph vessels.
Did you know?
Lymphatic vessels and blood vessels are similar in structure and function. Lymph is not actively pumped by the heart but is forced through the vessels by the movements of the body muscles.
Larger Lymphatic Vessels, Trunks, and Ducts
The lymphatic capillaries empty into larger lymphatic vessels, which are similar to veins in terms of their three-tunic structure and the presence of valves. These one-way valves are located fairly close to one another, and each one causes a bulge in the lymphatic vessel, giving the vessels a beaded appearance (see Figure 11.2).
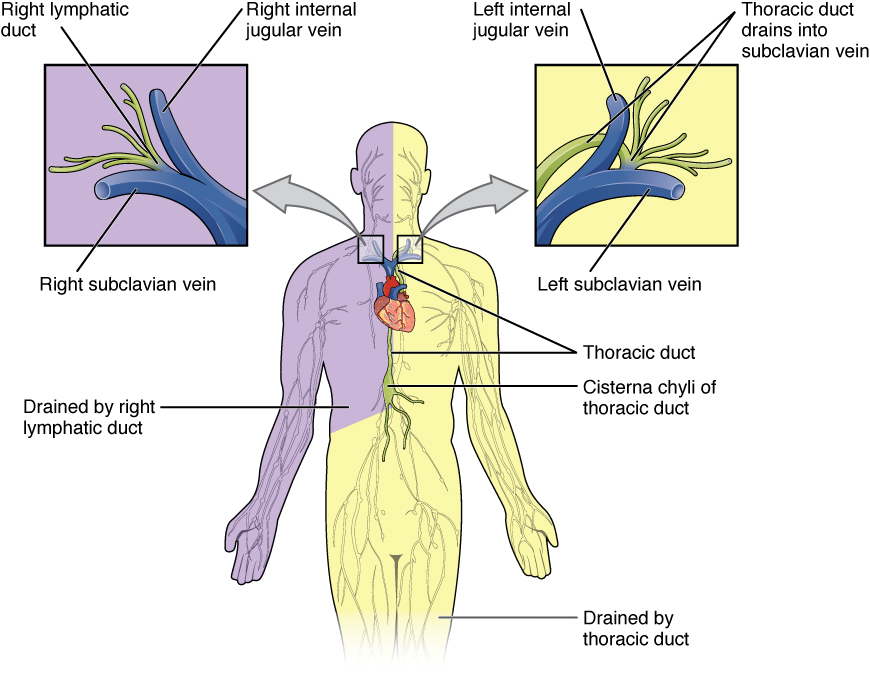
In general, superficial lymphatics follow the same routes as veins, whereas deep lymphatic vessels of the viscera generally follow the paths of arteries. The superficial and deep lymphatics eventually merge to form larger lymphatic structures known as the lymphatic trunks. On the right side of the body, the right sides of the head, thorax, and right upper limb trunks drain lymph fluid into the right subclavian vein via the right lymphatic duct (see Figure 11.3). On the left side of the body, the trunks from the remaining portions of the body drain into the larger thoracic duct, which drains into the left subclavian vein. The thoracic duct itself begins just beneath the diaphragm in the cisterna chyli.
Primary Lymphoid Organs
The primary lymphoid organs are the bone marrow and thymus gland. The lymphoid organs are where lymphocytes mature, proliferate, and are selected, which enables them to attack pathogens without harming the cells of the body.
- Bone Marrow
- Recall that all blood cells, including lymphocytes, are formed in the red bone marrow. The B cell undergoes nearly all of its development in the red bone marrow, whereas the immature T cell, called a thymocyte, leaves the bone marrow and matures largely in the thymus gland.
- Thymus
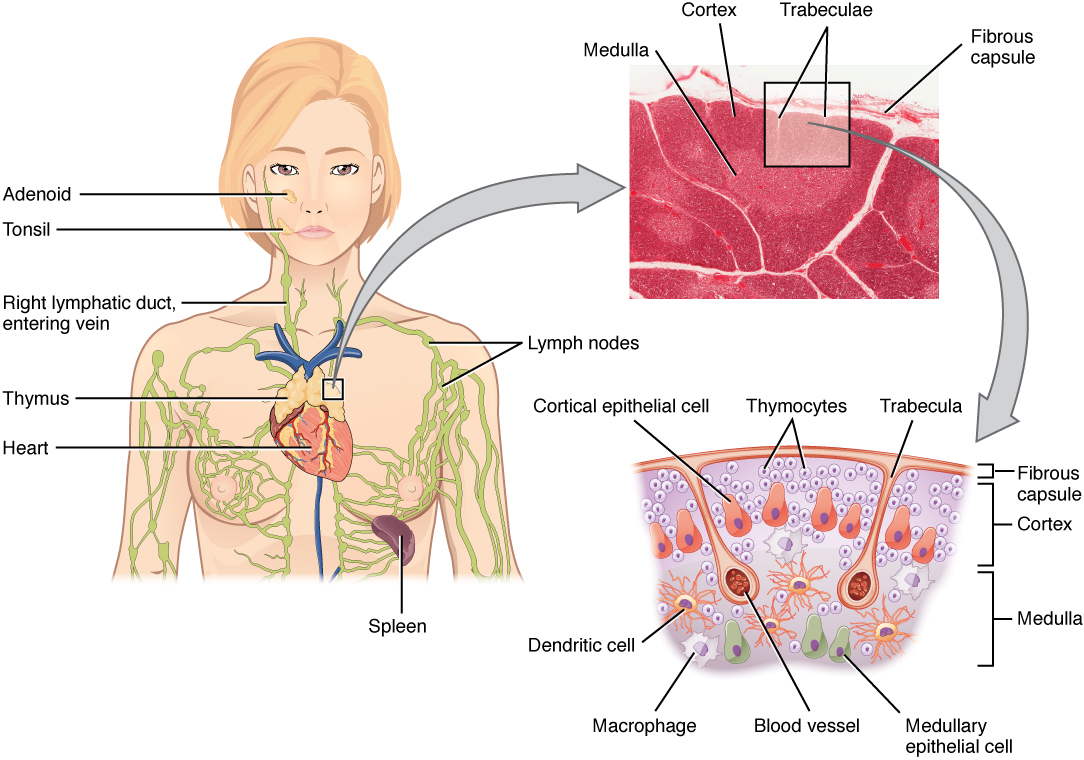
- The thymus gland, where T cells mature, is a bilobed organ found in the space between the sternum and the aorta of the heart (see Figure 11.4). Connective tissue holds the lobes closely together but also separates them and forms a capsule.
- The loss of immune function with age is called immunosenescence. One major cause of age-related immune deficiencies is thymic involution.
- The shrinking of the thymus gland begins at birth at a rate of about 3% tissue loss per year. This shrinking continues until 35 to 45 years of age when the rate declines to about 1% loss per year for the rest of one’s life. At that pace, the total loss of thymic epithelial tissue and thymocytes would occur at about 120 years of age. So, in theory, 120 years could be the maximum life span.
Concept Check
- Do you remember what the suffix “-oid” means?
- Can you explain the term lymphoid?
Secondary Lymphoid Organs
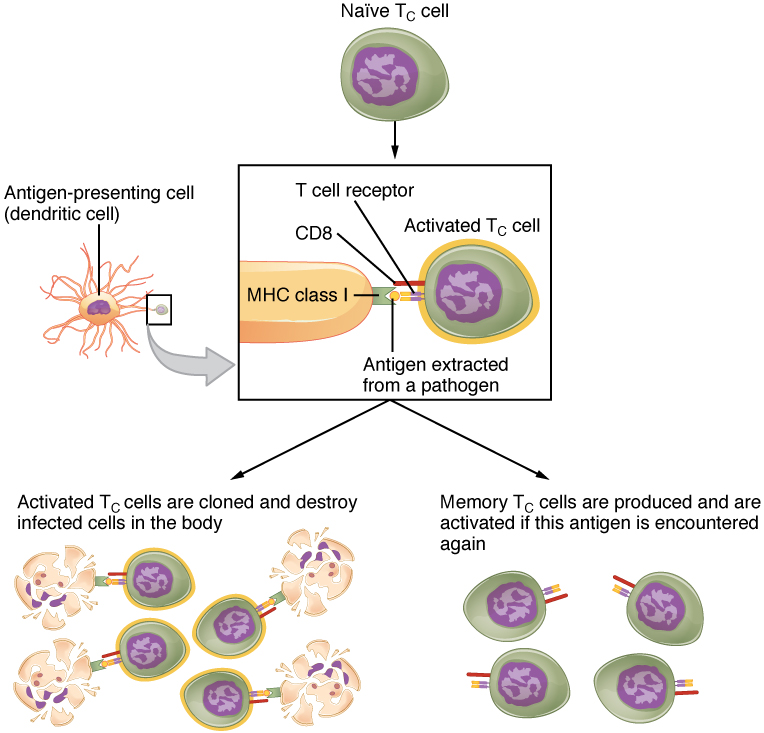
Lymphocytes develop and mature in the primary lymphoid organs, but they mount immune responses from the secondary lymphoid organs, which include the lymph nodes, spleen, and lymphoid nodules. A naïve lymphocyte is one that has left the primary organ, where it learned to function immunologically, and entered a secondary lymphoid organ where it waits to encounter an antigen against which it will mount a response (see Figure 11.5).
Did you know?
The thymus gland produces a hormone called thymosin and is therefore also considered to be part of the endocrine system.
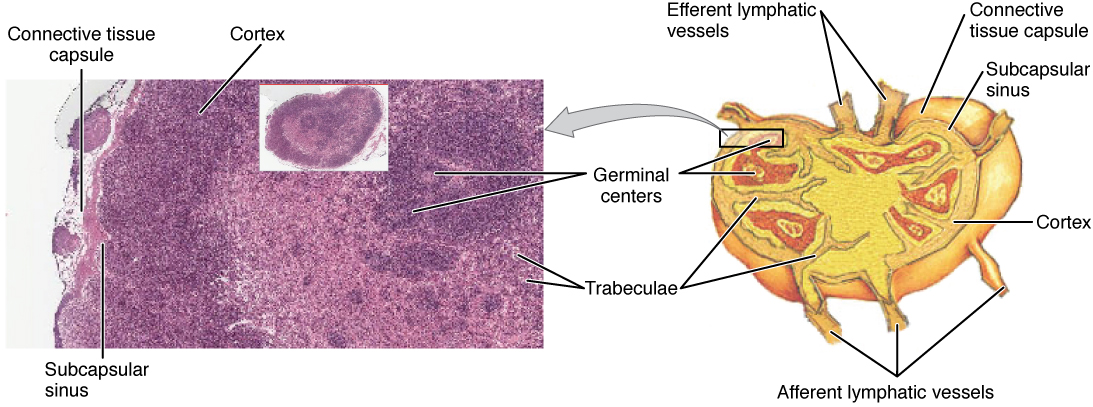
Lymph Nodes
Lymph nodes function to remove debris and pathogens from the lymph and are thus sometimes referred to as the “filters of the lymph” (see Figure 11.6). Any bacteria that infect the interstitial fluid are taken up by the lymphatic capillaries and transported to a regional lymph node. Dendritic cells and macrophages within this organ internalize and kill many of the pathogens that pass through, thereby removing them from the body. The lymph node is also the site of adaptive immune responses mediated by T cells, B cells, and accessory cells of the adaptive immune system.
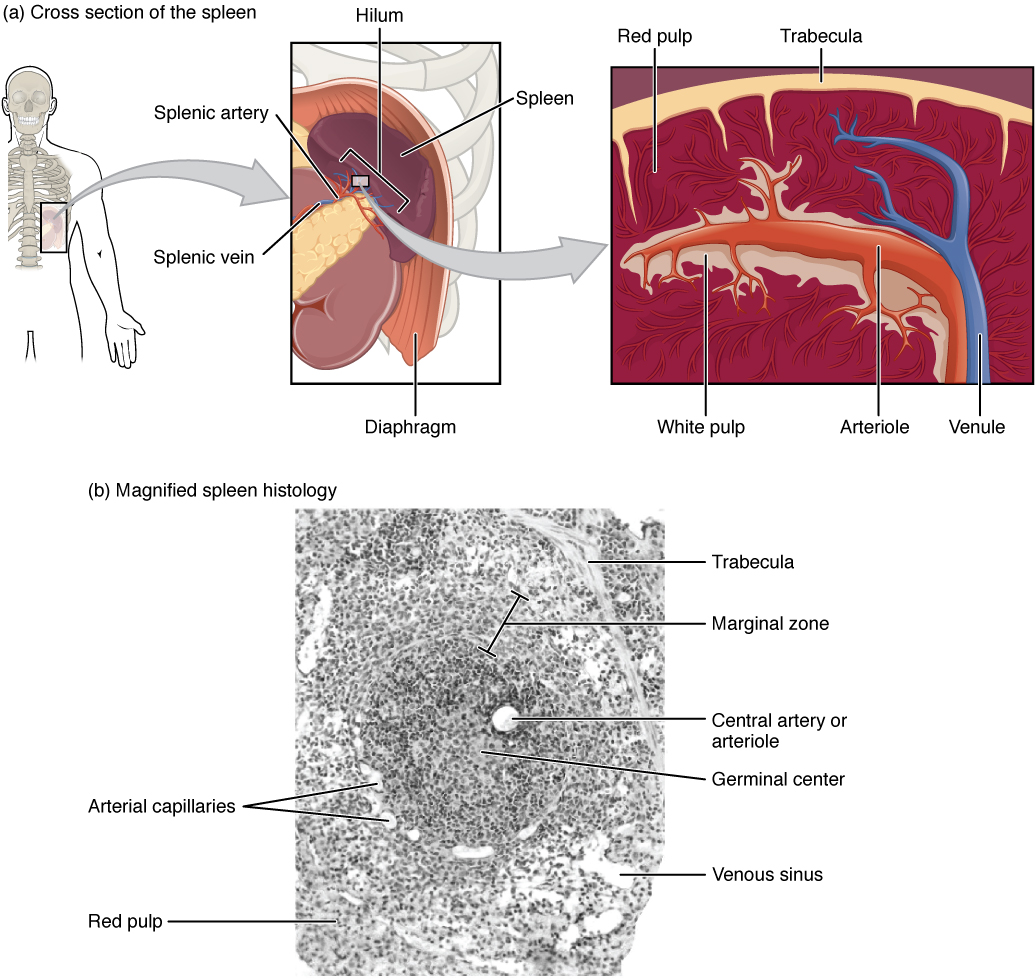
Spleen
The spleen is a vascular organ that is somewhat fragile due to the absence of a capsule. It is about 12 cm long and is attached to the lateral border of the stomach. The spleen is sometimes called the “filter of the blood” because of its extensive vascularization and the presence of macrophages and dendritic cells that remove microbes and other materials from the blood, including dying red blood cells. The spleen also functions as the location of immune responses to blood-borne pathogens.
Did you know?
You can live without your spleen. Do you remember the term for “surgical removal of the spleen”?
Lymphoid Nodules
The other lymphoid tissues, the lymphoid nodules, consist of a dense cluster of lymphocytes without a surrounding fibrous capsule. These nodules are located in the respiratory and digestive tracts, areas routinely exposed to environmental pathogens.
Tonsils are lymphoid nodules located along the inner surface of the pharynx and are important in developing immunity to oral pathogens (see Figure 11.8). The tonsil located at the back of the throat, the pharyngeal tonsil, is sometimes referred to as the adenoid when swollen. Such swelling is an indication of an active immune response to infection. Tonsils have deep grooves called crypts, which accumulate all sorts of materials taken into the body through eating and breathing and actually “encourage” pathogens to penetrate deep into the tonsillar tissues where they are eliminated. A major function of tonsils is to help children’s bodies recognize, destroy, and develop immunity to common environmental pathogens so that they will be protected in their later lives. Tonsils are often removed in children who have recurring throat infections since swollen palatine tonsils can interfere with breathing and/or swallowing.
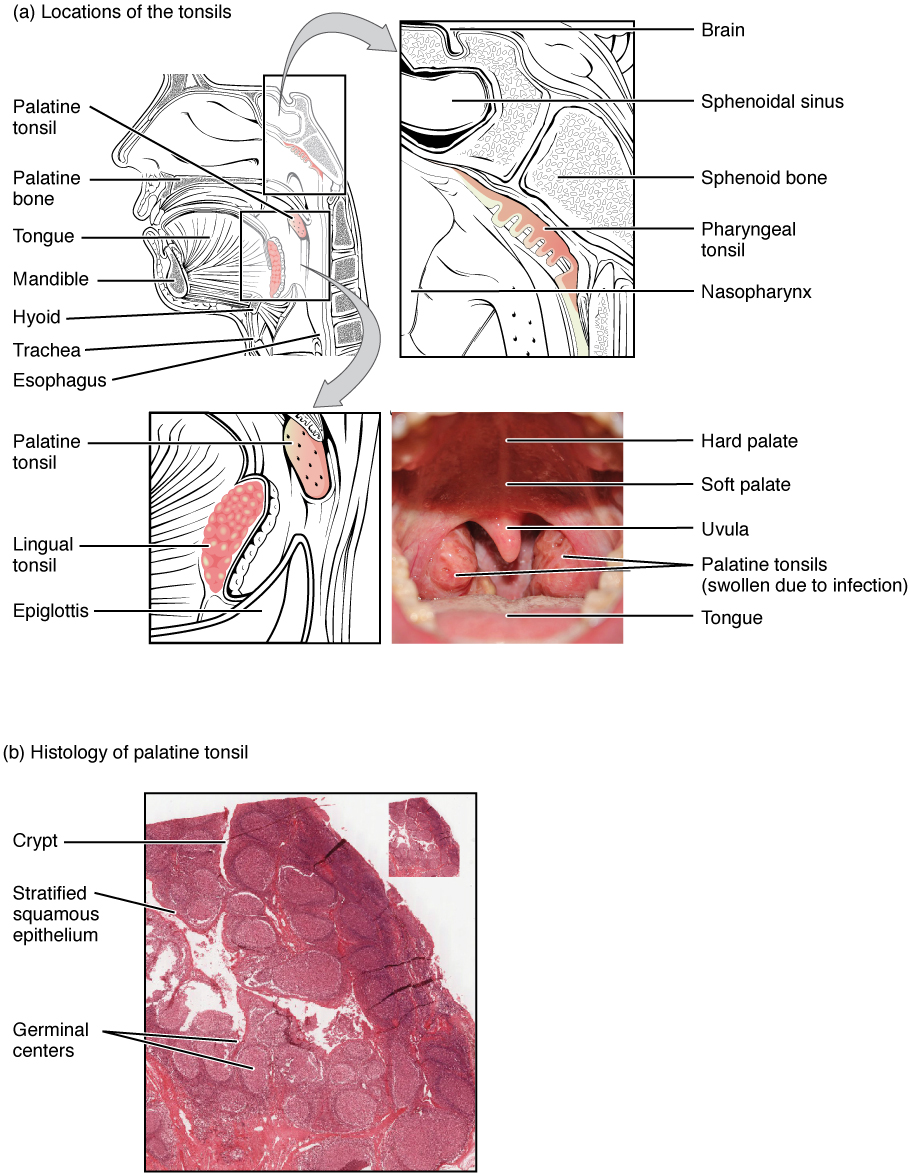
Concept Check
Tonsils are named after their locations.
- Look at the figure above and determine which anatomical structure is closely associated with each set of tonsils and was therefore used to name the tonsils, for example, the lingual tonsils are named after the tongue (lingula).
- Can you tell which structures were used to name the palatine tonsils and the pharyngeal tonsils?
Bronchus-associated lymphoid tissue (BALT) consists of lymphoid follicular structures with an overlying epithelial layer found along the bifurcations of the bronchi, and between bronchi and arteries. These tissues, in addition to the tonsils, are effective against inhaled pathogens.
Mucosa-associated lymphoid tissue (MALT) consists of an aggregate of lymphoid follicles directly associated with mucous membrane. MALT makes up dome-shaped structures found underlying the mucosa of the gastrointestinal tract, breast tissue, lungs, and eyes. Peyer’s patches, a type of MALT in the small intestine, are especially important for immune responses against ingested substances (see Figure 11.9). Peyer’s patches contain specialized cells that sample material from the intestinal lumen and transport it to nearby follicles so that adaptive immune responses to potential pathogens can be mounted.

The Organization of the Immune System
The immune system is a collection of barriers, cells, and soluble proteins that interact and communicate with each other in extraordinarily complex ways. The modern model of immune function is organized into a three-phase immune response (based on the timing of their effects). Ideally, this response will rid the body of a pathogen entirely (see Figure 11.10).
Think of a primary infection as a race between the pathogen and the immune system:
- The pathogen bypasses barrier defenses and starts to multiply in the host’s body.
- During the first 4 to 5 days, the innate immune response will partially control, but not stop the pathogen growth.
- The slower but more specific and effective adaptive immune response gears up and becomes progressively stronger, it will begin to clear the pathogen from the body. This clearance is referred to as seroconversion. It should be noted that seroconversion does not necessarily mean a patient is getting well.
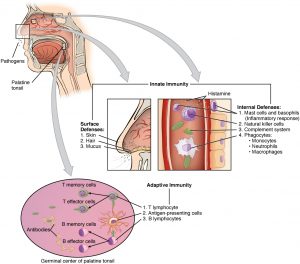
Phase 1: Barrier Defenses
Barrier defenses are part of the body’s most basic innate defense mechanisms. They are not a response to infections, but rather are continuously working to protect against pathogens by preventing them from entering the body, destroying them after they enter, or flushing them out before they can establish themselves.
Barrier defenses examples:
- Skin:
- Keratinized cells of the surface are too dry for bacteria to grow and are continuously sloughed off, along with pathogens that are on their surfaces.
- Skin (sweat glands, sebaceous glands):
- Lower pH than pathogens prefer, may contain substances that are toxic to pathogens, washing action.
- Oral Cavity (salivary glands):
- Lysozyme is an enzyme that destroys bacteria.
- Stomach:
- Low pH which is fatal to many pathogens.
- Mucosal:
- Traps both microbes and debris, and facilitates their removal.
- Normal flora (nonpathogenic bacteria):
- Prevents pathogens from growing on mucosal surfaces.
Phase 2: Innate Immune Response
Innate immune responses are critical to the early control of infections. Whereas barrier defenses are the body’s first line of physical defense against pathogens, innate immune responses are the first line of physiological defense. Innate responses occur rapidly, but with less specificity and effectiveness than the adaptive immune response. Within the first few days of an infection, a series of antibacterial proteins are induced, each with activities against certain bacteria. Additionally, interferons are induced that protect cells from viruses in their vicinity. Finally, the innate immune response does not stop when the adaptive immune response is developed. In fact, both can cooperate and one can influence the other in their responses against pathogens.
Innate immune responses (and early induced responses) are in many cases ineffective at completely controlling pathogen growth but they slow pathogen growth and allow time for the adaptive immune response to strengthen and either control or eliminate the pathogen. The innate immune system also sends signals to the cells of the adaptive immune system, guiding them in how to attack the pathogen.
Watch this video:
Media 11.2 Immune System, Part 1: Crash Course A&P #45 [Online video]. Copyright 2015 by CrashCourse.
Cells of the Innate Immune Response
Phagocytes: Macrophages and Neutrophils
A phagocyte is a cell that is able to surround and engulf a particle or cell, a process called phagocytosis. The phagocytes of the immune system engulf other particles or cells, either to clean an area of debris, old cells, or to kill pathogenic organisms such as bacteria. Macrophages, neutrophils, and dendritic cells are the major phagocytes of the immune system and are the body’s fast acting, front line immunological defense against organisms that have breached barrier defenses and have entered the body.
Macrophages not only participate in innate immune responses but have also evolved to cooperate with lymphocytes as part of the adaptive immune response. Macrophages exist in many tissues of the body, either freely roaming through connective tissues or fixed to reticular fibers within specific tissues such as lymph nodes. When pathogens breach the body’s barrier defenses, macrophages are the first line of defense.
A neutrophil is a phagocytic cell that is attracted via chemotaxis from the bloodstream to infected tissues. contains cytoplasmic granules, which in turn contain a variety of vasoactive mediators such as histamine. Whereas macrophages act like sentries, always on guard against infection, neutrophils can be thought of as military reinforcements that are called into a battle to hasten the destruction of the enemy.
A monocyte is a circulating precursor cell that differentiates into either a macrophage or dendritic cell, which can be rapidly attracted to areas of infection by signal molecules of inflammation.
Natural Killer (NK) Cells
Natural killer cells are a type of lymphocyte that have the ability to induce apoptosis in cells infected with pathogens such as intracellular bacteria and viruses. If apoptosis is induced before the virus has the ability to synthesize and assemble all its components, no infectious virus will be released from the cell, thus preventing further infection.
Soluble Mediators of the Innate Immune Response
Concept Check
Do you know the difference between these terms?
Cytokines and Chemokines
A cytokine is a signaling molecule that allows cells to communicate with each other over short distances. Cytokines are secreted into the intercellular space, and the action of the cytokine induces the receiving cell to change its physiology. A chemokine is a soluble chemical mediator similar to cytokines except that its function is to attract cells (chemotaxis) from longer distances.
Early Induced Proteins
Early induced proteins are those that are not constitutively present in the body but are made as they are needed early during the innate immune response. Interferons are an example of early induced proteins. Cells infected with viruses secrete interferons that travel to adjacent cells and induce them to make antiviral proteins. Thus, even though the initial cell is sacrificed, the surrounding cells are protected.
Inflammatory Response
The hallmark of the innate immune response is inflammation. Stub a toe, cut a finger, or do any activity that causes tissue damage and inflammation will result with its four characteristics: heat, redness, pain, and swelling (“loss of function” is sometimes mentioned as a fifth characteristic). It is important to note that inflammation does not have to be initiated by an infection, but can also be caused by tissue injuries. The release of damaged cellular contents into the site of injury is enough to stimulate the response, even in the absence of breaks in physical barriers that would allow pathogens to enter (by hitting your thumb with a hammer, for example). The inflammatory reaction brings in phagocytic cells to the damaged area to clear cellular debris and encourages the entry of clotting factors to set the stage for wound repair. Inflammation also facilitates the transport of antigen to lymph nodes by dendritic cells for the development of the adaptive immune response.
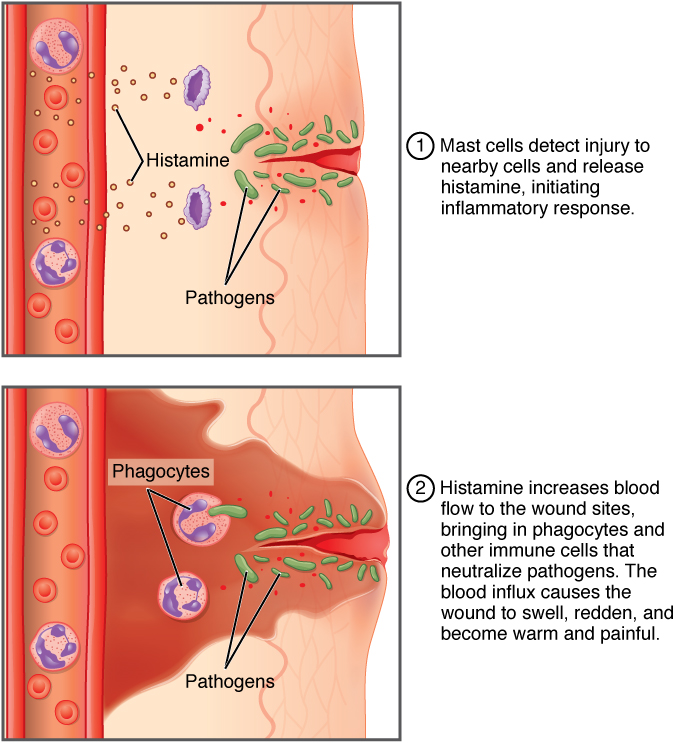
The above image summarizes the following events in the inflammatory response:
- The released contents of injured cells stimulate the release of substances from mast cells including histamine, leukotrienes, and prostaglandins.
- Histamine increases blood flow to the area by vasodilation, resulting in heat and redness. Histamine also increases the permeability of local capillaries, causing plasma to leak out and form interstitial fluid, resulting in swelling.
- Leukotrienes attract neutrophils from the blood by chemotaxis.
When local infections are severe, neutrophils are attracted to the sites of infections in large numbers, and as they phagocytose the pathogens and subsequently die, their accumulated cellular remains are visible as pus at the infection site. - Prostaglandins cause vasodilation by relaxing vascular smooth muscle and are a major cause of the pain associated with inflammation. Nonsteroidal anti-inflammatory drugs such as aspirin and ibuprofen relieve pain by inhibiting prostaglandin production.
Concept Check
- Do you remember the suffix used to describe ‘inflammation’?
- Describe what causes the pain associated with inflammation.
Acute inflammation is a short-term innate immune response to an insult to the body. If the cause of the inflammation is not resolved, however, it can lead to chronic inflammation, which is associated with major tissue destruction and fibrosis.
Phase 3: Adaptive Immune Response
Watch this video:
Media 11.3 Immune System, Part 2: Crash Course A&P #46 [Online video]. Copyright 2015 by CrashCourse.
Benefits of the Adaptive Immune Response
- Specificity
- The ability to specifically recognize and mount a response against almost any pathogen.
- Antigens are recognized by receptors on the surface of B and T lymphocytes.
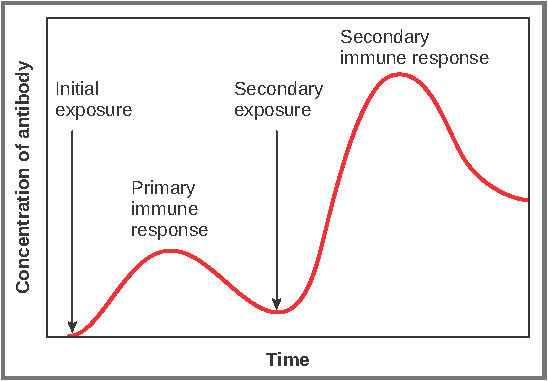
- Immunological Memory
- The first exposure to a pathogen is called a primary adaptive response.
- Symptoms of a first infection, called primary disease, are always relatively severe because it takes time for an initial adaptive immune response to a pathogen to become effective.
- Upon re-exposure to the same pathogen, a secondary adaptive immune response is generated, which is stronger and faster than the primary response, often eliminating the pathogen before it can cause damage or even symptoms.
- This secondary response is the basis of immunological memory, which gives us immunity.
- Self Recognition
- The ability to distinguish between self-antigens, those that are normally present in the body, and foreign antigens, those that might be on a potential pathogen.
- As T and B cells mature, there are mechanisms in place that prevent them from recognizing self-antigen, preventing a damaging immune response against the body. When these mechanisms fail, their breakdown leads to autoimmune diseases.
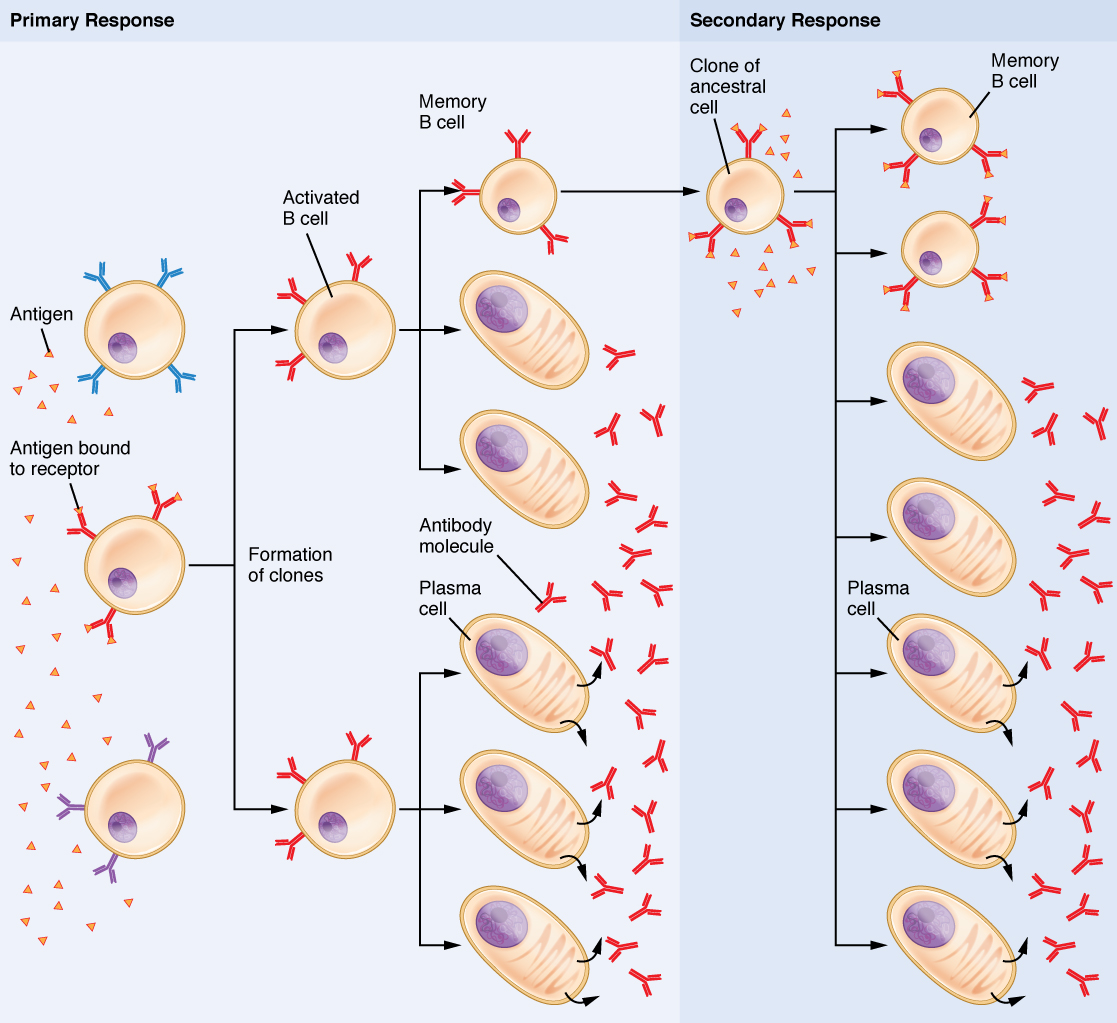
Lymphocytes: B Cells, T Cells, Plasma Cells
As stated above, lymphocytes are the primary cells of adaptive immune responses. These cells were introduced in the previous chapter and are summarized in the following table:
| CELL TYPE | DESCRIPTION AND DETAILS |
| Plasma Cell | B cell (lymphocyte) that has been activated through exposure to an antigen and produces antibodies against that antigen (see the figure below).
There are 5 classes of antibodies (IgM, IgG, IgE, IgA, IgD), each functioning in different ways: IgM promotes chemotaxis, opsonization, and cell lysis, making it a very effective antibody against bacteria at early stages of a primary antibody response IgG is the one that crosses the placenta to protect the developing fetus from disease and exits the blood to the interstitial fluid to fight extracellular pathogens IgA is the only antibody to leave the interior of the body to protect body surfaces. IgA is also of importance to newborns, because this antibody is present in mother’s breast milk (colostrum), which serves to protect the infant IgE is associated with allergies and anaphylaxis |
| T Cell | Different T cell types have the ability to either secrete soluble factors that communicate with other cells of the adaptive immune response or destroy cells infected with intracellular pathogen.
|
| Memory Cell | B cells and T cells formed during primary exposure to a pathogen (see the figure below).
Remain in the body for a long time after infection and are able to mount a fast and effective immune response to a pathogen if it is encountered a second time, preventing the pathogen from causing disease. |
Active Versus Passive Immunity
Immunity to pathogens, and the ability to control pathogen growth so that damage to the tissues of the body is limited, can be acquired by:
- The active development of an immune response in the infected individual; or
- The passive transfer of immune components from an immune individual to a non-immune one.
The downside to this passive immunity is the lack of the development of immunological memory. Once the antibodies are transferred, they are effective for only a limited time before they degrade.
| IMMUNITY | NATURAL | ARTIFICIAL |
|---|---|---|
| Active: resistance to pathogens acquired during an adaptive immune response | Result of memory cells formed during the adaptive immune response to a pathogen | Vaccine response. Through vaccination, one avoids the disease that results from the first exposure to the pathogen, yet reaps the benefits of protection from immunological memory. Vaccination was one of the major medical advances of the twentieth century and led to the eradication of smallpox and the control of many infectious diseases, including polio, measles, and whooping cough |
| Passive: transfer of antibodies from an immune person to a nonimmune person | Trans-placental antibodies from mother to fetus and maternal antibodies in breast milk protect newborn from infections | Immunoglobulin injections taken from animals previously exposed to a specific pathogen; a fast-acting method of temporarily protecting an individual who was possibly exposed to a pathogen |
Evasion of the Immune System by Pathogens
The immune system and pathogens are in a slow, evolutionary race to see who stays on top. Early childhood is a time when the body develops much of its immunological memory that protects it from diseases in adulthood. Pathogens have shown the ability, however, to evade the body’s immune responses, as described below.
-
- Protective adaptations: It is important to keep in mind that although the immune system has evolved to be able to control many pathogens, pathogens themselves have evolved ways to evade the immune response. An example is in Mycobacterium tuberculosis, which has evolved a complex cell wall that is resistant to the digestive enzymes of the macrophages that ingest them, and thus persists in the host, causing the chronic disease tuberculosis.
-
- Multiple strains: Bacteria sometimes evade immune responses because they exist in multiple strains, each having different surface antigens and requiring individual adaptive immune responses. One example is a small group of strains of S. aureus, called methicillin-resistant Staphylococcus aureus (MRSA), which has become resistant to multiple antibiotics.
-
- Antigen mutation: Because viruses’ surface molecules mutate continuously, viruses like influenza change enough each year that the flu vaccine for one year may not protect against the flu common to the next. New vaccine formulations must be derived for each flu season.
-
- Genetic recombination: An example is the influenza virus, which contains gene segments that can recombine when two different viruses infect the same cell. Recombination between human and pig influenza viruses led to the 2010 H1N1 swine flu outbreak.
-
- Immunosuppression: Pathogens, especially viruses, can produce immunosuppressive molecules that impair immune function.
Tissue Transplantation
One disease of transplantation occurs with bone marrow transplants, which are used to treat various diseases, including severe combined immunodeficiency disease (SCID) and leukemia. Because the bone marrow cells being transplanted contain lymphocytes capable of mounting an immune response, and because the recipient’s immune response has been destroyed before receiving the transplant, the donor cells may attack the recipient tissues, causing graft-versus-host disease. Signs and symptoms of this disease, which usually include a rash and damage to the liver and mucosa, are variable. Attempts have been made to moderate the disease by first removing mature T cells from the donor bone marrow before transplanting it.
Immune Responses Against Cancer
It is clear that with some cancers, like Kaposi’s sarcoma (see Figure 11.14), for example, that a healthy immune system does a good job at controlling them. This disease, which is caused by the human herpes virus, is almost never observed in individuals with strong immune systems. Other examples of cancers caused by viruses include liver cancer, caused by the hepatitis B virus, and cervical cancer, caused by the human papillomavirus. As these last two viruses have vaccines available for them, getting vaccinated can help prevent these two types of cancer by stimulating the immune response.

On the other hand, as cancer cells are often able to divide and mutate rapidly, they may escape the immune response, just as certain pathogens such as the human immunodeficiency virus (HIV) do.
There are three stages in the immune response to many cancers:
-
- Elimination occurs when the immune response first develops toward tumor-specific antigens specific to the cancer and actively kills most cancer cells.
- Equilibrium is the period that follows, during which the remaining cancer cells are held in check.
- Escape of the immune response, and resulting disease, occurs because many cancers mutate and no longer express any specific antigens for the immune system to respond to.
This fact has led to extensive research in trying to develop ways to enhance the early immune response to completely eliminate the early cancer and thus prevent a later escape. One method that has shown some success is the use of cancer vaccines. These differ from other vaccines in that they are directed against the cells of one’s own body. Treated cancer cells are injected into cancer patients to enhance their anti-cancer immune response and thereby prolong survival. The immune system has the capability to detect these cancer cells and proliferate faster than the cancer cells do, thus overwhelming the cancer in a similar way as they do for viruses. Cancer vaccines are being developed for malignant melanoma and renal (kidney) cell carcinoma.
Immune Responses and Stress
In order to protect the entire body from infection, the immune system is required to interact with other organ systems, sometimes in complex ways. For example, hormones such as cortisol (naturally produced by the adrenal cortex) and prednisone (synthetic) are well known for their abilities to suppress T cell immune mechanisms; hence, their prominent use in medicine as long-term, anti-inflammatory drugs.
One well-established interaction of the immune, nervous, and endocrine systems is the effect of stress on immune health. In the human vertebrate evolutionary past, stress was associated with the fight-or-flight response, largely mediated by the central nervous system and the adrenal medulla. This stress was necessary for survival since fighting or fleeing usually resolved the problem in one way or another. It has been found that short-term stress diverts the body’s resources towards enhancing innate immune responses. This has the ability to act fast and would seem to help the body prepare better for possible infections associated with the trauma that may result from a fight-or-flight exchange.
On the other hand, there are no physical actions to resolve most modern day stresses, including short-term stressors like taking examinations and long-term stressors such as being unemployed or losing a spouse. The effect of stress can be felt by nearly every organ system, and the immune system is no exception (see Table 11.3). Chronic stress, unlike short-term stress, may inhibit immune responses even in otherwise healthy adults. The suppression of both innate and adaptive immune responses is clearly associated with increases in some diseases.
| SYSTEM | STRESS-RELATED ILLNESS |
|---|---|
| Integumentary system | Acne, skin rashes, irritation |
| Nervous system | Headaches, depression, anxiety, irritability, loss of appetite, lack of motivation, reduced mental performance |
| Muscular and skeletal systems | Muscle and joint pain, neck and shoulder pain |
| Circulatory system | Increased heart rate, hypertension, increased probability of heart attacks |
| Digestive system | Indigestion, heartburn, stomach pain, nausea, diarrhea, constipation, weight gain or loss |
| Immune system | Depressed ability to fight infections |
| Male reproductive system | Lowered sperm production, impotence, reduced sexual desire |
| Female reproductive system | Irregular menstrual cycle, reduced sexual desire |
Anatomy Labeling Activity
Practice Terms Related to the Lymphatic and Immune Systems
Common Abbreviations for the Lymphatic and Immune Systems
Many terms and phrases related to the lymphatic and immune systems are abbreviated. Learn these common abbreviations by expanding the list below.
Diseases and Disorders of the Lymphatic and Immune Systems
The immune response can be under-reactive or over-reactive, leading to a state of disease. The factors that maintain immunological homeostasis are complex and incompletely understood.
Lymphedema
Lymphedema is a condition in which lymphatic fluid builds up in the body’s soft tissues. Lymphedema often occurs in the arms and legs, although other body parts may be affected. There are two types of lymphedema: primary and secondary. Primary lymphedema may be congenital and is caused by abnormalities in the lymph system. Secondary lymphedema occurs when the lymph system is damaged or blocked due to injury, cancer, or cancer treatment. Signs and symptoms include swelling of the limbs and digits, difficulty moving the joints in the arms and legs, and the sensation that the skin is too tight. Lymphedema is rarely cured. Instead, treatment such as the use of pressure garments, light exercise, massage therapy, and surgery can reduce symptoms and lower the risk of complications. Patients with severe cases of lymphedema are at an increased risk of developing lymphangiosarcoma, an aggressive cancer of the lymph vessels (National Cancer Institute, 2021; Sleigh & Manna, 2021). For more information, visit the Mayo Clinic’s web page on lymphedema.
Underactive Immune System: Immunodeficiencies
Suppressed immunity can result from inherited genetic defects or by acquiring viruses.
Inherited Immunodeficiencies/SCID
New treatments for SCID using gene therapy, inserting non-defective genes into cells taken from the patient and giving them back, have the advantage of not needing the tissue match required for standard transplants. Although not a standard treatment, this approach holds promise, especially for those in whom standard bone marrow transplantation has failed.
Acquired Immunodeficiency/HIV and AIDS
After seroconversion, the amount of virus circulating in the blood drops and stays at a low level for several years. During this time, the levels of CD4 T cells decline steadily, until at some point, the immune response is so weak that opportunistic disease and eventually death result.
Treatment for the disease consists of drugs that target virally encoded proteins that are necessary for viral replication but are absent from normal human cells. By targeting the virus itself and sparing the cells, this approach has been successful in significantly prolonging the lives of HIV-positive individuals.
Overactive Immune System: Hypersensitivities and Autoimmune Diseases
Hypersensitivities
| TYPE OF HYPERSENSITIVITY | DETAILS AND EXPLANATION |
| Type I |
|
| Type II |
|
| Type III |
|
| Type IV |
|
Autoimmune Responses
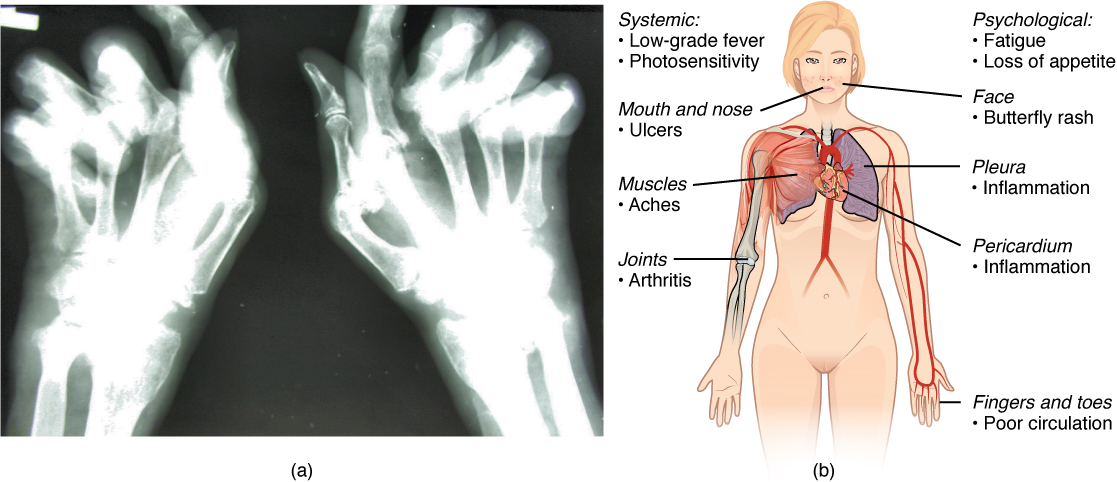
The worst cases of the immune system overreacting are autoimmune diseases in which the immune systems begin to attack cells of the patient’s own body, causing chronic inflammation and significant damage. The trigger for these diseases is often unknown, although environmental and genetic factors are likely involved. Treatments are usually based on resolving the symptoms using immunosuppressive and anti-inflammatory drugs. Figure 11.15 below provides two examples of autoimmune diseases: rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE).
Overall, there are more than 80 different autoimmune diseases, which are a significant health problem in the elderly. Table 11.5 below lists several of the most common autoimmune diseases, the antigens that are targeted (autoantigen or “self” antigen), and the resulting tissue damage.
| DISEASE | AUTOANTIGEN | SYMPTOMS |
|---|---|---|
| Celiac disease | Tissue transglutaminase | Damage to small intestine |
| Diabetes mellitus type I | Beta cells of pancreas | Low insulin production; inability to regulate serum glucose |
| Graves’ disease | Thyroid-stimulating hormone receptor (antibody blocks receptor) | Hyperthyroidism |
| Hashimoto’s thyroiditis | Thyroid-stimulating hormone receptor (antibody mimics hormone and stimulates receptor) | Hypothyroidism |
| Lupus erythematosus | Nuclear DNA and proteins | Damage of many body systems |
| Myasthenia gravis | Acetylcholine receptor in neuromuscular junctions | Debilitating muscle weakness |
| Rheumatoid arthritis | Joint capsule antigens | Chronic inflammation of joints |
Lymphoma
Lymphoma is a form of cancer in which masses of malignant T and/or B lymphocytes collect in lymph nodes, the spleen, the liver, and other tissues. As in leukemia, the malignant leukocytes do not function properly, and the patient is vulnerable to infection. Some forms of lymphoma tend to progress slowly and respond well to treatment. Others tend to progress quickly and require aggressive treatment, without which they are rapidly fatal.
Medical Terms in Context
Medical Specialties and Procedures Related to the Lymphatic and Immune Systems
Clinical immunologists and allergists diagnose and treat diseases of the immune system (National Center for O*Net Development, 2021). For more information, please visit the American Academy of Allergy, Asthma, and Immunology’s web page on careers in immunology.
Skin Testing
Skin testing (for allergies) is done by a clinical immunologist/allergist to identify allergens in Type I hypersensitivity. In skin testing, allergen extracts are injected into the epidermis, and a positive result of the wheal and flare response usually occurs within 30 minutes. The soft center is due to fluid leaking from the blood vessels and the redness is caused by the increased blood flow to the area that results from the dilation of local blood vessels at the site.
Lymphatic and Immune Systems Vocabulary
-
-
-
- Active immunity
Immunity developed from an individual’s own immune system.
Acute inflammation
Inflammation occurring for a limited time period; rapidly developing.
Adaptive immune response
A relatively slow but very specific and effective immune response controlled by lymphocytes.
Afferent lymphatic vessels
Vessels that lead into a lymph node.
Allergens
Antigens that evoke type 1 hypersensitivity (allergy) responses.
Allergist
Specialist who specializes in treating individuals with a hypersensitivity to allergens.
Allergy
Inflammatory response due to a hypersensitivity to a substance that normally is harmless or would not cause an immune response in most people.
Anaphylactic shock
A severe and sometimes life-threatening immune system reaction to an antigen that a person has been previously exposed to. The reaction may include itchy skin, edema, collapsed blood vessels, fainting, difficulty in breathing, and death.
Antibody
A protein made by plasma cells (a type of white blood cell) in response to an antigen (a substance that causes the body to make a specific immune response). Each antibody can bind to only one specific antigen. The purpose of this binding is to help destroy the antigen.
Antigens
Substances that provokes an immune response. This happens because the immune system sees the antigen as foreign, or ‘non-self” (does not belong in that body).
Apoptosis
Programmed cell death.
Autoimmune diseases/disorders
Disorders in which the immune system overreacts and begins to attack itself.
B cells
Lymphocytes that act by differentiating into an antibody-secreting plasma cell.
Barrier defenses
Antipathogen defenses deriving from a barrier that physically prevents pathogens from entering the body to establish an infection.
Bone marrow
Tissue found inside bones; the site of all blood cell differentiation and maturation of B lymphocytes.
Bronchus-associated lymphoid tissue (BALT)
Lymphoid nodule associated with the respiratory tract.
CD4 T Cells
CD4 is the receptor that HIV uses to get inside T cells and reproduce. CD4+ helper T cells play an important role in T cell immune responses and antibody responses.
Chemokine
Soluble, long-range, cell-to-cell communication molecule.
Chemotaxis
Movement in response to chemicals; a phenomenon in which injured or infected cells and nearby leukocytes emit the equivalent of a chemical “911” call, attracting more leukocytes to the site.
Chronic inflammation
Ongoing inflammation that can be caused by foreign bodies, persistent pathogens, and autoimmune diseases such as rheumatoid arthritis.
Chyle
Lipid-rich lymph inside the lymphatic capillaries of the small intestine.
Cisterna chyli
A sac-like chamber that receives lymph from the lower abdomen, pelvis, and lower limbs by way of the left and right lumbar trunks and the intestinal trunk.
Complement
Enzymatic cascade of constitutive blood proteins that have antipathogen effects, including the direct killing of bacteria.
Cytokine
A signaling molecule that allows cells to communicate with each other over short distances.
Deep lymphatic vessels
Lymphatic vessels of the organs.
Efferent lymphatic vessels
Vessels that lead out of a lymph node.
Erythroblastosis fetalis
An immune reaction between maternal and fetal blood due to the Rh antigen; also known as hemolytic disease of the newborn (HDN).
Genetic recombination
The combining of gene segments from two different pathogens.
Graft-versus-host disease (GVHD)
A condition that can occur in bone marrow transplant recipients; occurs when the transplanted cells mount an immune response against the recipient’s tissue.
Histamine
A vasodilator involved in the inflammatory response.
Human immunodeficiency virus (HIV)
An infectious disease transmitted through semen, vaginal fluids, and blood that suppresses the immune system. HIV infection may be managed with antiviral drugs or may progress to acquired immune deficiency syndrome (AIDS).
Hypersensitivities
Reacting to something that would not normally evoke a reaction.
Immune system
Series of barriers, cells, and soluble mediators that combine to response to infections of the body with pathogenic organisms.
Immunity
Resistant to the effects of pathogens.
Immunodeficiency
The decreased ability of the body to fight infections and other diseases.
Immunological memory
Ability of the adaptive immune response to mount a stronger and faster immune response upon re-exposure to a pathogen.
Immunology
The study of the body’s immune system.
Induration
A firm, raised reddened patch of skin.
Inflammation
Basic innate immune response characterized by heat, redness, pain, and swelling.
Innate immune response
Fast-acting non-specific immune mechanisms that are present from birth.
Intercellular
Between cells.
Interferons
Early induced proteins made in virally infected cells that cause nearby cells to make antiviral proteins.
Interstitial fluid
Extracellular fluid not contained within blood vessels.
Interstitial space
Spaces between individual cells in the tissues.
Intracellular
Inside the cell membrane or within the cell.
Leukemia
A cancer involving an abundance of leukocytes.
Lymph
The term used to describe interstitial fluid once it has entered the lymphatic system.
Lymph node
One of the bean-shaped organs found associated with the lymphatic vessels.
Lymphatic capillaries
Smallest of the lymphatic vessels and the origin of lymph flow.
Lymphatic system
Network of lymphatic vessels, lymph nodes, and ducts that carries lymph from the tissues and back to the bloodstream.
Lymphatic trunks
Large lymphatics that collect lymph from smaller lymphatic vessels and empties into the blood via lymphatic ducts.
Lymphocytes
The second most common type of leukocyte and are essential for the immune response.
Lymphoid nodules
Unencapsulated patches of lymphoid tissue found throughout the body.
Lymphoma
A form of cancer in which masses of malignant T and/or B lymphocytes collect in lymph nodes, the spleen, the liver, and other tissues. These leukocytes do not function properly, and the patient is vulnerable to infection.
Macrophage
A large cell derived from a monocyte; they participate in innate immune responses.
Major histocompatibility complex (MHC)
Protein structures found on the outside of cells that help the immune system recognize non-self antigens.
Mast cell
Cell found in the skin and the lining of body cells that contains cytoplasmic granules with vasoactive mediators such as histamine.
Memory T cells
Long-lived immune cells reserved for future exposure to a pathogen.
Monocyte
A type of immune cell that is made in the bone marrow.
Mucosa-associated lymphoid tissue (MALT)
Lymphoid nodule associated with the mucosa.
Mucous membranes
Epithelial membranes that line the body cavities and hollow passageways that open to the external environment.
Naïve lymphocyte
Mature B or T cell that has not yet encountered antigen for the first time.
Natural killer cell (NK)
Cytotoxic lymphocyte of innate immune response.
Neutrophil
Phagocytic white blood cell recruited from the bloodstream to the site of infection via the bloodstream.
Opsonization
A process by which an antibody or an antimicrobial protein binds to a pathogen, thereby marking it as a target for phagocytes.
Passive immunity
Transfer of immunity to a pathogen to an individual that lacks immunity to this pathogen usually by the injection of antibodies.
Pathogen
An organism that causes a disease.
Phagocytosis
Movement of material from the outside to the inside of the cells via vesicles made from invaginations of the plasma membrane; process where some white blood cells engulf invading microorganisms.
Plasma cells
A type of B lymphocyte that produces antibodies, which bind to specific foreign or abnormal antigens in order to destroy them.
Primary adaptive response
Immune system’s response to the first exposure to a pathogen.
Primary lymphoid organs
Site where lymphocytes mature and proliferate; for example, red bone marrow and the thymus gland.
Right lymphatic duct
Drains lymph fluid from the upper right side of the body into the right subclavian vein.
Staphylococcus aureus
A bacteria that is commonly found in minor skin infections, as well as in the nose of some healthy people.
Secondary adaptive response
Immune response observed upon re-exposure to a pathogen, which is stronger and faster than a primary response.
Secondary lymphoid organs
Sites where lymphocytes mount adaptive immune responses, examples include lymph nodes and spleen.
Seroconversion
The reciprocal relationship between virus levels in the blood and antibody levels.
Severe combined immunodeficiency disease (SCID)
A rare, inherited disease that is marked by a lack of B and T lymphocytes.
Spleen
Secondary lymphoid organ that filters pathogens from the blood (white pulp) and removes degenerating or damaged blood cells (red pulp).
Superficial lymphatics
Lymphatic vessels of the subcutaneous tissues of the skin.
Systemic lupus erythematosus (SLE)
A chronic, inflammatory, connective tissue disease that can affect the joints and many organs; also called lupus.
T cell
Lymphocyte that acts by secreting molecules that regulate the immune system or by causing the destruction of foreign cells, viruses, and cancer cells.
Thoracic duct
Large duct that drains lymph from the lower limbs, left thorax, left upper limb, and the left side of the head.
Thymocytes
A type of white blood cell that is part of the immune system and develops from stem cells in the bone marrow; also called T cells and T lymphocytes.
Thymus
Primary lymphoid organ, where t lymphocytes proliferate and mature.
Tissue typing
The determination of major histocompatibility complex (MHC) molecules in the tissue to be transplanted to better match the donor to the recipient.
Tonsils
Lymphoid nodules associated with the nasopharynx.
Vaccine
A killed or weakened pathogen or its components that, when administered to a healthy individual, leads to the development of immunological memory (a weakened primary immune response) without causing much in the way of symptoms.
Vasodilation
The physiological widening of blood vessels by relaxing the vascular smooth muscle.
Wheal and flare response
A soft, pale swelling at the site surrounded by a red zone.
Test Yourself
References
CrashCourse. (2015, November 30). Lymphatic system: Crash course A&P #44 [Video]. YouTube. https://youtu.be/I7orwMgTQ5I
CrashCourse. (2015, December 8). Immune system, part 1: Crash course A&P #45 [Video]. YouTube. https://youtu.be/GIJK3dwCWCw
CrashCourse. (2015, December 14). Immune system, part 2: Crash course A&P #46 [Video]. YouTube. https://youtu.be/2DFN4IBZ3rI
National Center for O*NET Development. (2021) 29-1229.01 – Allergists and Immunologists. O*NET OnLine. Retrieved November 2, 2021, from https://www.onetonline.org/link/summary/29-1229.01
National Cancer Institute. (2021). Lymphedema (PDQ®)–Patient version. National Institutes of Health. https://www.cancer.gov/about-cancer/treatment/side-effects/lymphedema/lymphedema-pdq
Sleigh, B. C., & Manna, Bi. (2021). Lymphedema. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537239/
Image Descriptions
Figure 11.1 image description: The left panel shows a female human body, and the entire lymphatic system is shown Labels read (clockwise from top): thymus, lymph nodes, thymus, spleen, lymph vessel, bone marrow, right lymphatic duct, entering vein, tonsil, adenoid. The right panel shows magnified images of the thymus and the lymph node. Labels read (clockwise from top): tissue cell, interstitial fluid, lymphatic capillary, blood capillary, lymphatic vessel. Label of lymph node reads masses of lymphocytes and macrophages. [Return to Figure 11.1].
Figure 11.2 image description: This image shows the lymph capillaries in the tissue spaces. Labels read (clockwise, from top): lymph capillary, tissue cells, venule, lymphatic vessel, tissue fluid, arteriole). It also shows a magnified image showing the interstitial fluid and the lymph vessels. Labels read (clockwise, from top): collagen fiber, interstitial fluid, lymph, lymph vessel endothelial cells, backflow prevention valve, endothelial flaps. [Return to Figure 11.2].
Figure 11.3 image description: This figure shows the lymphatic trunks and the duct system in the human body. Labels read (clockwise from top) thoracic duct, cisterna chyli of thoracic duct, drained by thoracic duct, drained by right lymphatic duct. Callouts to the left and right show the magnified views of the left and right jugular vein respectively. Labels read (right lymphatic duct): right internal jugular vein, right subclavian vein, right lymphatic duct; (left jugular vein): left internal jugular vein, thoracic duct drains into subclavian vein, left subclavian vein.[Return to Figure 11.3].
Figure 11.4 image description: The left panel of this figure shows the head and chest of a woman and the location of the thymus is marked. Labels read (clockwise, from top) lymph nodes, spleen, heart, thymus, right lymphatic duct entering vein, tonsil, adenoid. The top right panel shows a micrograph of the thymus. Labels read (from left to right): medulla, cortex, trabeculae, fibrous capsule. The bottom right panel shows a magnified view of the structure of the thymus. Labels read (clockwise, from top): thymocytes, trabecula, fibrous capsule, cortex, medulla (layers), medullary epithelial cell, blood vessel, macrophage, dendritic cell, cortical epithelial cell.[Return to Figure 11.4].
Figure 11.5 image description:This flowchart shows the process in which a naïve T cell becomes activated T cells in the left part of the pathway and memory cells in the right part of the pathway. A naive T cell becomes an activated T cell when an antigen-presenting cell is introduced. The antigen is extracted from a pathogen and then either activated T cells are cloned and destroy the infected cells in the body, and/or memory T cells are produced and are activated if this antigen is encountered again. [Return to Figure 11.5].
Figure 11.6 image description: The left panel of this figure shows a micrograph of the cross section of a lymph node. Labels indicate the connective tissue capsule, cortex, and subcapsular sinus. The right panel shows the structure of a lymph node. Labels indicate (from top, clockwise) the efferent lymphatic vessels, connective tissue capsule, subcapsular sinus, cortex, afferent lymphatic vessels, trabecula, and germinal centers. [Return to Figure 11.6].
Figure 11.7 image description: The top left panel shows the location of the spleen in the human body. The top center panel shows a close up view of the location of the spleen. Labels read (clockwise, from top): hilum, spleen, diaphragm, splenic vein, splenic artery. The top right panel shows the blood vessels and spleen tissue. Labels read (from left to right, top then bottom) red pulp, trabecula (bottom) white pulp, arteriole, venule. The bottom panel shows a histological micrograph Labels read (clockwise, from top): trabecula, marginal zone, central artery or arteriole, germinal center, venous sinus, red pulp, arterial capillaries. [Return to Figure 11.7].
Figure 11.8 image description: The top panel of this image shows the locations of the tonsils. Labels read (clockwise from top):palatine tonsil, palatine bone, tongue, mandible, hyoid, trachea, esophagus. Callout shows the location of the pharyngeal tonsil. Labels read (from top): brain, sphenoidal sinus, sphenoid bone, pharyngeal tonsil, nasopharynx. Another callout details the location of the palatine tonsil. Labels read (from top): palatine tonsil, lingual tonsil, epiglottis. Another callout shows a photograph of the back of the throat where the tonsils are located. Labels read (from top) hard palate, soft palate, uvula, palatine tonsils (swollen due to infection) and tongue. The bottom panel shows the histological micrograph of the tonsils. Labels read (from top): crypt, stratified squamous epithelium, germinal centers. [Return to Figure 11.8].
Figure 11.9 image description: This figure shows a micrograph of a mucosa associated lymphoid tissue (MAST) nodule. Labels indicate the mucosa and Peyer’s patches (which appear to be dark purple). [Return to Figure 11.9].
Figure 11.10 image description: This figure shows a lateral view of a human face in the top left. A magnified callout shows the germinal center of the palatine tonsil. Another magnified view shows how the innate immune system works. This process is described in greater detail in the text below the figure. [Return to Figure 11.10].
Figure 11.11 image description: The top panel of this figure shows the mast cells detecting an injury and initiating an inflammatory response. The bottom panel shows the increase in blood flow in response to histamine. [Return to Figure 11.11].
Figure 11.12 image description: This graph shows the antibody concentration as a function of time in primary and secondary response. Initial exposure indicates a low concentration of antibody, which then elevates over time during the primary immune response. It decreases a little during secondary exposure, but then spikes during the secondary immune response. [Return to Figure 11.12].
Figure 11.13 image description: This flowchart shows how the clonal selection of B cells takes place. The left panel shows the primary response and the right panel shows the secondary response. During a primary B cell immune response, both antibody-secreting plasma cells and memory B cells are produced. These memory cells lead to the differentiation of more plasma cells and memory B cells during secondary responses. [Return to Figure 11.13].
Figure 11.14 image description: This image shows Kaposi’s Sarcoma lesions on the surface of the skin. [Return to Figure 11.14].
Figure 11.15 image description: The left panel of this figure shows an x-ray image of a person’s hand with rheumatoid arthritis, and the right panel of this figure shows a woman’s body with labels showing the different responses in the body when the patient suffers from lupus. Labels (from top, clockwise) read: psychological: fatigue, loss of appetite, face butterfly rash, pleura inflammation, pericardium inflammation, fingers and toes poor circulation, joints arthritis, muscles aches, mouth and nose ulcers, systemic: low-grade fever photosensitivity.[Return to Figure 11.15].
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts et al. and is used under a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
- Active immunity
-
-
The term used to describe interstitial fluid once it has entered the lymphatic system (Betts et al., 2013)
Spaces between individual cells in the tissues (Betts et al., 2013)
The term given to extracellular fluid not contained within blood vessels (Betts et al., 2013)
Lymphatic vessels of the subcutaneous tissues of the skin (Betts et al., 2013)
Lymphatic vessels of the organs (Betts et al., 2013)
Large lymphatic vessels that collect lymph from smaller lymphatic vessels and empty it into the blood via lymphatic ducts (Betts et al., 2013)
A sac-like chamber that receives lymph from the lower abdomen, pelvis, and lower limbs by way of the left and right lumbar trunks and the intestinal trunk (Betts et al, 2013)
The shrinking of the thymus due to age (Betts et al., 2013)
A type of white blood cell that is part of the immune system and develops from stem cells in the bone marrow; also called T cells and T lymphocytes (National Cancer Institute, n.d.)
Site where lymphocytes mature and proliferate; for example, red bone marrow and the thymus gland (Betts et al., 2013)
A relatively slow but very specific and effective immune response controlled by lymphocytes (Betts et al., 2013)
Antipathogen defenses deriving from a barrier that physically prevents pathogens from entering the body to establish an infection (Betts et al., 2013)
Fast-acting non-specific immune mechanisms that are present from birth (Betts et al., 2013)
The reciprocal relationship between virus levels in the blood and antibody levels (Betts et al., 2013)
A measure of how acidic or alkaline a substance is, as determined by the number of free hydrogen ions in the substance (Betts et al., 2013)
Epithelial membranes that line the body cavities and hollow passageways that open to the external environment (Betts et al., 2013)
Early induced proteins made in virally infected cells that cause nearby cells to make antiviral proteins (Betts et al., 2013)
Cells that engulf and absorb bacteria and cell particles (Betts et al., 2013)
Programmed cell death (Betts et al., 2013)
Between cells (Betts et al., 2013)
Inside the cell membrane or within the cell (Betts et al., 2013)
Extracellular fluid not contained within blood vessels (Betts et al., 2013)
The physiological widening of blood vessels by relaxing the vascular smooth muscle (National Library of Medicine, 2021)
Movement in response to chemicals; a phenomenon in which injured or infected cells and nearby leukocytes emit the equivalent of a chemical “911” call, attracting more leukocytes to the site (Betts et al., 2013)
Ongoing inflammation that can be caused by foreign bodies, persistent pathogens, and autoimmune diseases such as rheumatoid arthritis (Betts et al., 2013)
A substance that provokes an immune response. This happens because the immune system sees the antigen as foreign, or 'non-self" (does not belong in that body) (Betts et al., 2013)
Pertaining to the body's ability to mount an overwhelming immune response against a pathogen so that it cannot produce disease (Betts et al., 2013)
A protein made by plasma cells (a type of white blood cell) in response to an antigen (a substance that causes the body to make a specific immune response). Each antibody can bind to only one specific antigen. The purpose of this binding is to help destroy the antigen (National Cancer Institute, n.d.)
A process by which an antibody or an antimicrobial protein binds to a pathogen, thereby marking it as a target for phagocytes (Betts et al., 2013)
A severe and sometimes life-threatening immune system reaction to an antigen that a person has been previously exposed to. The reaction may include itchy skin, edema, collapsed blood vessels, fainting, difficulty in breathing, and death (National Cancer Institute, n.d.)
chemical that sends a message from one cell to another
A killed or weakened pathogen or its components that, when administered to a healthy individual, leads to the development of immunological memory (a weakened primary immune response) without causing much in the way of symptoms (Betts et al., 2013)
A bacteria that is commonly found in minor skin infections, as well as in the nose of some healthy people (Betts et al., 2013)
The combining of gene segments from two different pathogens (Betts et al., 2013)
The determination of major histocompatibility complex (MHC) molecules in the tissue to be transplanted to better match the donor to the recipient (Betts et al., 2013)
Protein structures found on the outside of cells that help the immune system recognize non-self antigens (Betts et al., 2013)
A rare, inherited disease that is marked by a lack of B and T lymphocytes (National Cancer Institute, n.d.)
A cancer involving an abundance of leukocytes (Betts, et al., 2013)
A condition that can occur in bone marrow transplant recipients; occurs when the transplanted cells mount an immune response against the recipient's tissue (Betts et al., 2013)
Finger or toe (Betts et al., 2013)
An infectious disease transmitted through semen, vaginal fluids, and blood that suppresses the immune system. HIV infection may be managed with antiviral drugs or may progress to acquired immune deficiency syndrome (AIDS) (Betts et al., 2013)
CD4 is the receptor that HIV uses to get inside T cells and reproduce. CD4+ helper T cells play an important role in T cell immune responses and antibody responses. (Betts et al., 2013)
Reacting to something that would not normally evoke a reaction (Betts et al., 2013)
Antigens that evoke type 1 hypersensitivity (allergy) responses (Betts et al., 2013)
An immune reaction between maternal and fetal blood due to the Rh antigen; also known as hemolytic disease of the newborn (HDN) (Betts et al., 2013)
A chronic, inflammatory, connective tissue disease that can affect the joints and many organs; also called lupus (National Cancer Institute, n.d.)
A firm, raised reddened patch of skin (Betts et al., 2013)
A form of cancer in which masses of malignant T and/or B lymphocytes collect in lymph nodes, the spleen, the liver, and other tissues. These leukocytes do not function properly, and the patient is vulnerable to infection (Betts. et al., 2013)
A soft, pale swelling at the site surrounded by a red zone (Betts et al., 2013)

