16 Male Reproductive System
Learning Objectives
- Examine the anatomy of the male reproductive system
- Determine the main functions of the male reproductive system
- Differentiate male reproductive system medical terms and common abbreviations
- Recognize the medical specialties associated with the male reproductive system
- Discover common diseases, disorders, and procedures related to the male reproductive system
Male Reproductive System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Male Reproductive System.
Introduction to the Male Reproductive System
Gametes are the reproductive cells that combine to form a fetus. Organs called gonads produce the gametes, along with the hormones that regulate human reproduction. The male gametes are called sperm. Spermatogenesis occurs within the seminiferous tubules that make up most of the testis. The scrotum is a sac that holds the testes outside of the body cavity.
Watch this video:
Media 16.1. Reproductive System, Part 2 – Male Reproductive System: Crash Course A&P 41 [Online video]. Copyright 2015 by CrashCourse.
Practice Medical Terms Related to the Male Reproductive System
Anatomy (Structures) of the Male Reproductive System
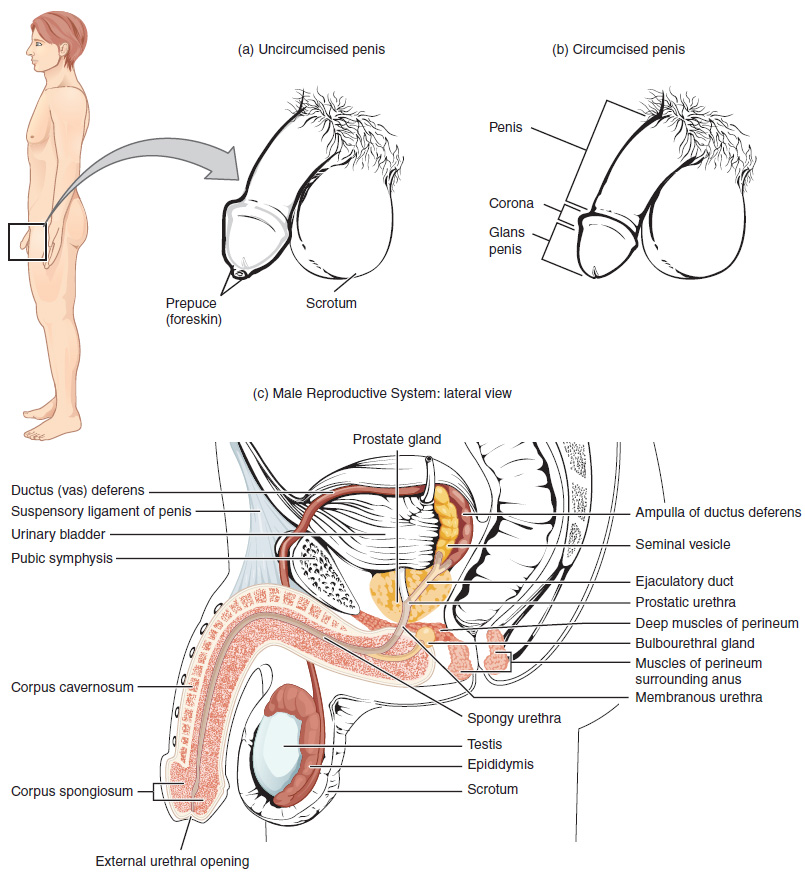
The structures of the male reproductive system include the testes, the epididymis, the penis, and the ducts and glands that produce and carry semen. Sperm exit the scrotum through the vas deferens. The spermatic cord is an enclosed sheath which includes the vas deferens, arteries, veins and nerves. The seminal vesicles and prostate add fluids to the sperm to create semen.
Physiology (Function) of the Male Reproductive System
Spermatogenesis
Spermatogenesis occurs in the seminiferous tubules that form the bulk of each testis. The process begins at puberty, after which time sperm is produced constantly throughout a man’s life. One production cycle takes approximately 64 days. One production cycle is considered from spermatogonia through to formed sperm. A new cycle starts approximately every 16 days, although this timing is not synchronous across the seminiferous tubules.
Sperm
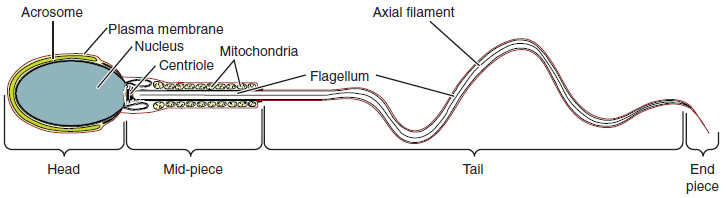
Sperm is smaller than most cells in the body; in fact, the volume of a sperm cell is 85,000 times less than that of the female gamete. Approximately 100 to 300 million sperm are produced each day, whereas women typically ovulate only one oocyte per month as is true for most cells in the body, the structure of sperm cells speaks to their function. Sperm have a distinctive head, mid-piece, and tail region (see Figure 16.2).
Sperm Transport
To fertilize an egg, sperm must be moved from the seminiferous tubules in the testes, through the epididymis, and—later during ejaculation—along the length of the penis and out into the female reproductive tract. It takes an average of 12 days for sperm to move through the coils of the epididymis, with the shortest recorded transit time in humans being one day.
Did you know?
Sperm counts slowly decline after age 35, and some studies suggest that smoking can lower sperm counts irrespective of age.
Epididymis
Sperm enter the head of the epididymis and are moved by the contraction of smooth muscles lining the epididymal tubes. As the sperm mature they acquire the ability to move under their own power. Once inside the female reproductive tract, they will use this ability to move independently toward the unfertilized egg. The more mature sperm are then stored in the tail of the epididymis until ejaculation occurs.
Ducts
During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle contraction to the vas deferens (also called the ductus deferens). The vas deferens is a thick, muscular tube that is bundled together inside the scrotum with connective tissue, blood vessels, and nerves into a structure called the spermatic cord. From each epididymis, each vas deferens extends through the inguinal canal in the abdominal wall and continues to a region called the ampulla. The sperm is mixed with fluid from the paired seminal vesicles and moves into its associated ejaculatory duct. The ejaculatory ducts transport the seminal fluid to the prostate gland.
Prostate Gland
The prostate gland secretes an alkaline, milky fluid to the passing seminal fluid (referred to as semen) to first coagulate and then decoagulate the semen following ejaculation. The temporary thickening of semen helps retain it within the female reproductive tract. Once decoagulated, the sperm can pass farther into the female reproductive tract.
Bulbourethral Glands
Bulbourethral glands release a thick, salty fluid that lubricates the end of the urethra and vagina, and helps to clean urine residues from the penile urethra.
Concept Check
- Write or draw out the components of the pathway that sperm takes from the beginning until the end.
- Consider fertility challenges that may be experienced if a large number of defective sperm are produced.
Anatomy Labeling Activity
Practice Terms Related to the Male Reproductive System
Common Abbreviations for the Male Reproductive System
Many terms and phrases related to the male reproductive system are abbreviated. Learn these common abbreviations by expanding the list below.
Diseases and Disorders of the Male Reproductive System
Erectile Dysfunction Disorder (EDD)
Erectile dysfunction (ED) is a condition in which a male has difficulty either initiating or maintaining an erection. The combined prevalence of minimal, moderate, and complete ED is approximately 40% in men at age 40 and reaches nearly 70% by 70 years of age. In addition to aging, ED is associated with diabetes, vascular disease, psychiatric disorders, prostate disorders, the use of some drugs such as certain antidepressants, and problems with the testes resulting in low testosterone concentrations. These physical and emotional conditions can lead to disruptions in the vasodilation pathway and result in an inability to achieve an erection.
Cancer
Prostate Cancer
According to the Centers for Disease Control and Prevention (CDC), prostate cancer is the second most common cancer occurring in men. However, some forms of prostate cancer grow very slowly and may not require treatment. Aggressive forms of prostate cancer, in contrast, involve metastasis to organs like the lungs and brain. There is no link between Benign Prostatic Hyperplasia (BPH) and prostate cancer, but the symptoms are similar. Prostate cancer is detected by medical history, a blood test, and a digital rectal exam that allows physicians to palpate the prostate and check for unusual masses. If a mass is detected, the cancer diagnosis is confirmed by biopsy of the cells (Betts et al., 2013; Centers for Disease Control, n.d-a.).
Testicular Cancer
Testicular cancer begins in the testicle or testis. It is most often found in men aged 20 to 35 years old, although it can occur at any age. Common signs and symptoms include a painless lump in the testicle, swelling, and a build-up of fluid in the scrotum. Testicular cancer is treatable when diagnosed early. An orchiectomy may be required for diagnosing and treating testicular cancer (National Cancer Institute, 2021a). For more information, visit the Cleveland Clinic’s web page on testicular cancer.
Did you know?
Family history is a common risk factor for testicular cancer.
Sexually Transmitted Infections and Diseases (STIs and STDs)
Although the terms sexually transmitted infections (STI) and sexually transmitted diseases (STD) are often used interchangeably, they have distinct meanings. STIs refer to infections caused by a virus, bacteria, fungus, or parasite via sexual contact. STDs refer to the disease state that develops as a result of infection (U.S. Department of Health and Human Services, 2020).
Chlamydia
Chlamydia is one of the most common sexually transmitted diseases. It is caused by the bacteria Chlamydia trachomatis, which infects the urethra and prostate in men. Chlamydia spreads through unprotected oral, anal, or vaginal sex with an infected person. Many people with chlamydia do not have any symptoms and unknowingly pass the infection to their sexual partner(s). If symptoms develop, they may not appear for several weeks after sexual contact with an infected person. Males may have penile discharge, itching around the urethra, and pain in or swelling of the testicles. Chlamydia is easy to treat with antibiotics and can be cured. However, until a patient finishes their treatment, they continue to have the infection and can continue to pass it to others (Centers for Disease Control and Prevention, n.d.-b).
Gonorrhea (Gonococcus)
Gonorrhea is a sexually transmitted disease caused by the bacterium Neisseria gonorrhoeae. It infects the mucous membranes of the reproductive tract, including the urethra in men. Infections can also infect the mouth, throat, eyes, and anus. Gonorrhea is spread through unprotected oral, vaginal or anal sex with an infected person. Many people infected with gonorrhea have no symptoms and can unknowingly pass the infection on to their sexual partner(s). Symptoms vary depending on which part of the body is infected. Males may have yellowish-white discharge from the penis or dysuria. Gonorrhea infection from oral sex may lead to a sore throat, whereas infection from anal sex may cause itchiness and discharge from the anus. Gonorrhea can be treated and cured with antibiotics in combination with an intramuscular (IM) injection. However, until the patient finishes their treatment, they continue to have the infection and can pass it to others (Centers for Disease Control and Prevention, n.d.-c).
Notifiable and Reportable Diseases
In every state in the United States, chlamydia and gonorrhea are notifiable and reportable diseases. This means that when a person tests positive for either of the STIs, public health departments and the CDC are informed so that they may monitor trends, identify outbreaks, and take the necessary steps to prevent further spread of the disease (Centers for Disease Control and Prevention, n.d.-d, n.d.-e).
Human Papillomavirus (HPV)
Human papillomavirus (HPV) is another common STI. Both males and females can be infected with HPV. There are over 200 strains of HPV. Some strains can cause visible genital warts, while others cause genital, anal, throat, and cervical cancers. HPV spreads through sexual activity and skin-to-skin contact in the genital area with an infected person. Since some people are asymptomatic, they don’t know they have the virus and consequently pass the virus to their sexual partners. Treatments are available for genital warts, but there is no cure for HPV. However, in the United States, a vaccine called Gardasil® 9 is available, which prevents infection with HPV (MedlinePlus, 2021; National Cancer Institute, 2021b). For more information, visit the Centers for Disease Control and Prevention’s web page on HPV.
Herpes Simplex Virus (HSV)
Genital herpes is a sexually transmitted disease that is caused by a virus called the herpes simplex virus (HSV). There are two types of herpes simplex viruses:
- Type 1- oral herpes or cold sores (HSV-1)
- Type 2- genital herpes (HSV-2)
Signs and symptoms might include dysuria, enlarged glands, myalgia, and fever. Once a patient is infected with HSV, the virus remains in their body even after the symptoms are gone and can cause recurring outbreaks. When the virus becomes active again, the symptoms return but are usually less painful and heal faster (Centers for Disease Control and Prevention, n.d.-f).
Herpes is spread through direct contact with the sores or blisters of an infected person. Contact (and transfer of the virus) can occur from genitals-to-genitals, mouth-to-genitals, or mouth-to-mouth. Herpes can also be passed to the anal area. Herpes spreads easily during sexual contact while symptoms are present or just before an outbreak of symptoms. An infected person may spread herpes even when they have no symptoms; this is called asymptomatic shedding. One can spread the herpes virus to other parts of their body after touching the sores. The fingers, eyes, and other body areas can accidentally become infected in this way. Hand washing after touching sores and blisters is recommended to prevent spreading the virus (Centers for Disease Control and Prevention, n.d.-f).
There is no cure for herpes. Antiviral pills help to reduce symptoms and speed the healing of blisters or sores and are prescribed by a doctor. All sexual partner(s) should be informed. The only way to reduce the risk of transmission of herpes is to avoid direct contact with the sores and to use condoms. Condoms will reduce but not eliminate risk, as the virus can be present and shed from the skin in the genital area (Centers for Disease Control and Prevention, n.d.-f).
Common Abbreviations for Reproductive Sexually Transmitted Infections (STIs)
Medical Terms in Context
Medical Specialties and Procedures Related to the Male Reproductive System
Urology
Urology is a specialty that focuses on the diagnosis, treatment, and surgical repair of the urinary tract. To learn more about urology as a specialty, visit the American College of Surgeons’ web page.
Vasectomy
A vasectomy is a procedure in which a small section of the ductus (vas) deferens is removed from the scrotum. This cuts off the path taken by sperm through the ductus deferens. Although it can be reversed, clinicians consider it permanent and advise men to undergo it only if they are certain that they no longer wish to father children. For more information, view this video from MedlinePlus on vasectomies.
Male Reproductive Vocabulary
Ablation
The removal or destruction of a body part or tissue or its function. Ablation may be performed by surgery, hormones, drugs, radiofrequency, heat, or other methods.
Arthralgia
Joint pain.
Aspermia
Condition of the complete absence of sperm.
Balanitis
Inflammation of the glans penis.
Benign prostatic hyperplasia (BPH)
A benign condition in which an overgrowth of prostate tissue pushes against the urethra and the bladder, blocking the flow of urine.
Bulbourethral glands
Glands that secrete a lubricating mucus that cleans and lubricates the urethra prior to and during ejaculation; also called Cowper’s glands.
Circumcision
The surgical removal of the prepuce.
Coitus
Sexual intercourse between a male and female.
Condom
A sheath that is worn over the penis during sexual behavior in order to prevent pregnancy or spread of sexually transmitted disease.
Corpus cavernosum
Either of two columns of erectile tissue in the penis that fill with blood during an erection.
Corpus spongiosum
Column of erectile tissue in the penis that fills with blood during an erection and surrounds the penile urethra on the ventral portion of the penis.
Cryptorchidism
The failure of one or both testes to descend into the scrotum prior to birth.
Ductus deferens
Duct that transports sperm from the epididymis through the spermatic cord and into the ejaculatory duct; also referred to as the vas deferens.
Dysuria
Painful urination.
Ejaculatory duct
Duct that connects the ampulla of the ductus deferens with the duct of the seminal vesicle at the prostatic urethra.
Enucleation
Excision of a whole organ or mass without cutting into it.
Epididymis
A coiled tubular structure in which sperm start to mature and are stored until ejaculation.
Epididymitis
Inflammation of the epididymis.
Gamete
A specialized sex cell carrying 23 chromosomes.
Glans penis
Bulbous end of the penis that contains a large number of nerve endings.
Gonadotropin-releasing hormone (GnRH)
Hormone released by the hypothalamus that regulates the production of follicle-stimulating hormone and luteinizing hormone from the pituitary gland.
Gonads
Reproductive organs (testes in men and ovaries in women) that produce gametes and reproductive hormones.
Hydrocele
Accumulation of serous fluid between the layers of membrane covering the testis.
Infertility
The inability to produce children.
Inguinal canal
Opening in the abdominal wall that connects the testes to the abdominal cavity.
Leydig cells
Cells between the seminiferous tubules of the testes that produce testosterone; a type of interstitial cell.
Myalgia
Pain in a muscle or group of muscles.
Oligospermia
Condition of a suboptimal concentration of spermatozoa in the ejaculated semen to ensure successful fertilization of an ovum.
Orchidectomy
Surgery to remove one or both testicles; also called orchiectomy.
Orchiectomy
Surgery to remove one or both testicles; also called orchidectomy.
Orchiopexy
Surgical fixation of the testicle.
Orchitis
Inflammation of a testis.
Penis
Male organ of copulation.
Polyuria
Excessive urine production.
Prepuce
Flap of skin that forms a collar around, and thus protects and lubricates, the glans penis; also referred to as the foreskin.
Prostate gland
A gland at the base of the bladder surrounding the urethra that contributes fluid to semen during ejaculation.
Prostatitis
Inflammation of the prostate gland.
Scrotum
An external pouch of skin and muscle that houses the testes.
Semen
Ejaculatory fluid composed of sperm and secretions from the seminal vesicles, prostate, and bulbourethral glands.
Seminal vesicle
Gland that produces seminal fluid, which contributes to semen.
Seminiferous tubules
Structures within the testes where spermatogenesis occurs.
Sertoli cells
Cells that support germ cells through the process of spermatogenesis; a type of sustentacular cell.
Sperm
Male gamete.
Spermatic cord
Bundle of nerves and blood vessels that supplies the testes; contains ductus deferens.
Spermatid
Immature sperm cells produced by meiosis II of secondary spermatocytes.
Spermatocyte
A male gametocyte from which a spermatozoon develops.
Spermatogenesis
The process of producing sperm.
Spermatogonia
The diploid precursor cells that become sperm.
Spermiogenesis
Transformation of spermatids to spermatozoa during spermatogenesis.
Sterility
A condition of being unable to produce children.
Testes
Male gonads.
Urethritis
Inflammation of the urethra.
Varicocele
Distended veins of the spermatic cord.
Vasectomy
A procedure in which a small section of the ductus deferens is cut and sealed to interrupt sperm delivery. It is an effective form of male birth control.
Vasovasostomy
Creation of an artificial opening between ducts to restore fertility to males who have had a vasectomy.
Test Yourself
References
Centers for Disease Control and Prevention. (n.d.-a). Prostate cancer statistics. https://www.cdc.gov/cancer/prostate/statistics/index.htm
Centers for Disease Control and Prevention. (n.d.-b). Chlamydia – CDC fact sheet (Detailed).
https://www.cdc.gov/std/chlamydia/stdfact-chlamydia-detailed.htm
Centers for Disease Control and Prevention. (n.d.-c). Gonorrhea – CDC fact sheet (Detailed). https://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea-detailed.htm
Centers for Disease Control and Prevention. (n.d.-d). Reporting and confidentiality. https://www.cdc.gov/std/treatment-guidelines/clinical-reporting.htm
Centers for Disease Control and Prevention. (n.d.-e). What is case surveillance? https://www.cdc.gov/nndss/about/index.html
Centers for Disease Control and Prevention. (n.d.-f). Genital herpes fact sheet. https://www.cdc.gov/std/herpes/stdfact-herpes.htm
CrashCourse. (2015, November 9). Reproductive system, part 2 – Male reproductive system: Crash course A&P 41. YouTube. https://youtu.be/-XQcnO4iX_U
MedlinePlus. (2021). HPV. U.S. National Library of Medicine. https://medlineplus.gov/hpv.html
National Cancer Institute. (2021a). Testicular cancer treatment (PDQ®)-Patient version. National Institutes of Health, U.S. Department of Health and Human Services. https://www.cancer.gov/types/testicular/patient/testicular-treatment-pdq
National Cancer Institute. (2021b). Human papillomavirus (HPV) vaccines. National Institutes of Health, U.S. Department of Health and Human Services. https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-vaccine-fact-sheet
U.S. Department of Health and Human Services. (2020). Sexually transmitted infections National Strategic Plan for the United States: 2021-2025. https://www.hhs.gov/sites/default/files/STI-National-Strategic-Plan-2021-2025.pdf
Image Descriptions
Figure 16.1 image description: This figure shows the different organs in the male reproductive system. The top panel shows the side view of a man and an uncircumcised and a circumcised penis. The bottom panel shows the lateral view of the male reproductive system and the major parts are labeled. [Return to Figure 16.1].
Figure 16.2 image description: This diagram shows the structure of sperm; the major parts are labeled (from left to right): head section (acrosome, plasma membrane, nucleus), mid-piece (centriole, mitochondria, flagellum), tail (flagellum, axial filament), end piece (end piece). [Return to Figure 16.2].
A specialized sex cell carrying 23 chromosomes (Betts et al., 2013)
Reproductive organs (testes in men and ovaries in women) that produce gametes and reproductive hormones (Betts et al., 2013)
The process of producing sperm (Betts et al., 2013)
Structures within the testes where spermatogenesis occurs (Betts et al., 2013)
An external pouch of skin and muscle that houses the testes (Betts et al., 2013)
Male gonads (Betts et al., 2013)
A blood vessel that transports blood away from the heart (Betts et al., 2013)
Blood vessels that conduct blood toward the heart (Betts et al., 2013)
Bundle of fibers that receives and sends messages between the body and the brain (National Cancer Institute, n.d.)
A gland at the base of the bladder surrounding the urethra that contributes fluid to semen during ejaculation (Betts et al., 2013)
Male gamete (spermatozoon) (Betts et al., 2013)
Ejaculatory fluid composed of sperm and secretions from the seminal vesicles, prostate, and bulbourethral glands (Betts et al., 2013)
The diploid precursor cells that become sperm (Betts et al., 2013)
Immature egg cell (Betts et al., 2013)
A coiled tubular structure in which sperm start to mature and are stored until ejaculation (Betts et al., 2013)
The duct that transports sperm from the epididymis through the spermatic cord and into the ejaculatory duct; also referred as the vas deferens (Betts et al., 2013)
Glands that secrete a lubricating mucus that cleans and lubricates the urethra prior to and during ejaculation; also called Cowper’s glands (Betts et al., 2013)
The process in which cancer spreads from one part of the body to another (Betts et al., 2013)
Male gonad (Betts et al., 2013)
Surgery to remove one or both testicles; also called orchidectomy (National Cancer Institute, n.d.)
Painful urination (National Library of Medicine, 2021)
pertaining to within the muscle
Having no signs or symptoms of disease (National Cancer Institute, n.d.)
Pain in a muscle or group of muscles (National Cancer Institute, n.d.)

