PSYCHIATRIC EMERGENCIES
This module aligns with key elements of APNA’s “Growth & Development”, “Clinical Decision Making”, and “Health Care Settings” (American Psychiatric Nurses Association Education Council, Undergraduate Branch, 2022).
Module Outline
- Assessment of Psychiatric Emergencies
- Problems Associated with Psychiatric Emergencies
- Treatment of Psychiatric Emergencies
Module Learning Outcomes
- Define and identify types of crises
- Identify the common nursing problems associated with Psychiatric Emergencies
- Summarize the treatment of Psychiatric Emergencies
Concepts
- Behavior
- Coping
- Safety
- Legal Issues
Overview
In this module, we will discuss matters related to psychiatric emergencies including their clinical presentation, assessment, and treatment variations. Rhoads (2021) indicates a psychiatric emergency involves thoughts, feelings, or actions that require immediate therapeutic intervention. Some examples of psychiatric emergencies include:
- Suicide
- Agitated/aggressive patients
- Rape
- Disaster
- Panic attack
- Delirium
- Neuroleptic malignant syndrome (NMS)
- Serotonin syndrome
- Overdose and withdrawal (Rhoads,2021).
Our discussion will consist of types of crises, suicide, aggression/violence, and abuse/neglect. Prior to discussing these clinical disorders, we will explain crises, as well as identify common crisis types.
Crises
Crises are individualistic and can relate to a positive or negative event that creates stress. Some individuals may be able to manage a crisis, provided they have access to sufficient resources (e.g., adaptive coping mechanisms, social support, financial means, insurance, and community organizations). However, if an individual is experiencing multiple stressors and/or crises, they may not successfully manage a crisis. As the adage advises, an ounce of prevention is worth a pound of cure. Specific to a crisis or psychiatric emergency, it is best to have a plan. Videbeck (2020) indicates specific types of crises generally fall into three categories:
- Maturational or developmental crises (e.g., leaving home, marriage, having a baby)
- Situational or unanticipated/sudden events (e.g., death of a loved one, job loss, physical/emotional illness)
- Adventitious or social crises (e.g., natural disasters, terrorist attacks, and violent crimes)
Three factors typically influence an individual’s experience of a crisis.
- Perception of the event
- Emotional support availability
- Coping mechanism availability (Videbeck, 2020).
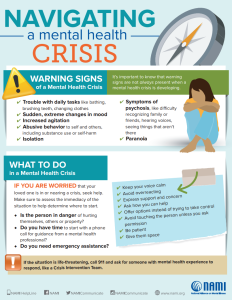
NAMI (2022b) provides several resources for navigating crises; these will be featured in this module. The first of these resources is below “Navigating a Mental Health Crisis” (2022b).
Below is an overview of a nurse’s consideration for the assessment, problems, and treatment of psychiatric emergencies.
See NAMI’s Resource “Navigating a Mental Health Crisis” (2022b), Thomas and Reeves(2022), and Carlson (2022) for further reading.
Assessment
Nurses should consider two key components when assessing an individual experiencing a psychiatric emergency.
- Ensure the safety of everyone involved, including the nurse’s safety, patient safety, and safety of others in the environment
- Attempt to identify the specific situation/event leading to the crisis
Suicide
An individual’s expression of suicidal ideation should always be taken seriously and requires immediate intervention. In many acute clinical settings, it is routine practice to ask each patient about suicidal or homicidal thoughts on admission and daily with each set of vital signs. Videbeck (2020) provides a list of suicide myths. Let’s summarize these myths.
Summarization of Suicide Myths
| Myth | Facts |
| People who talk about suicide, do not act on suicidal thoughts. | Individuals often communicate suicidal ideation and inner feelings of helplessness/hopelessness; these should always be taken seriously. |
| Individuals who talk about suicide will only hurt themselves. | Individuals may hurt themselves, but may also, impulsively or plan, hurt others. |
| You can’t help someone who wants to hurt themselves. | Individuals may have mixed feelings about suicide and hurting others. Intervention can most certainly help individuals get the help they need. |
| Mentioning “suicide” promotes the idea of suicide to the individual. | Asking about suicide does not cause an individual, who is not suicidal, to become a suicide risk. |
| Ignoring or challenging expressed suicidal thoughts will result in a reduction of actual suicide behaviors. | Suicidal gestures should never be ignored, challenged, or dismissed. All expressions of suicide should be taken seriously and require immediate intervention. Inquire about the situation that is prompting the suicidal thoughts. The person may feel relieved that help is imminent. |
| Individuals, who were a suicide risk, will always be a suicide risk. | Individuals, who complete suicide, typically have attempted suicide in the past. However, proper support and adaptive coping mechanisms can help individuals with suicidal ideation learn to become emotionally secure and learn adaptive ways to resolve problems. |
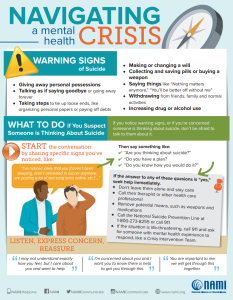
See NAMI’s (2022b) resource below for warning signs of crisis and interventions.
Aggression and Violence
Anger is a normal human emotion. However, when anger leads to aggression and violence, this becomes a situation requiring immediate intervention and de-escalation. Rhoads (2021) provides a list of behaviors indicative of warning signs that may lead to violence. Some of these behaviors include:
- Tense or angry facial expressions
- Restlessness, body tension, or pacing
- Increased speech volume and erratic movements
- Prolonged eye contact
- Withdrawal or refusal to communicate
- Violent-themed delusions or hallucinations
- Verbal threats or violent gestures
- Verbalization of anger or violent feelings.
Abuse and Neglect
Abuse involves acts of commission (e.g., physical, sexual, verbal, emotional) and neglect involves acts of omission (e.g., physical, medical, education, social, emotional) (Heldt, 2021). Nurses should be aware of warning signs of abuse and neglect. Carefully read over the summarization table below created from Videbeck’s (2020) resource. This table is not exhaustive.
Warning Signs of Abuse and Neglect
| Child | Elder |
| Serious injuries with no trauma history | Frequent injuries and seeking medical assistance at several locations |
| Delay in seeking treatment | Reluctance to seek treatment or denial of injury |
| Provided injury history is inconsistent with the severity of the injury | Disorientation or grogginess (possible misuse of medications) |
| Inconsistency or change to child history during evaluation | Fear or nervousness around family members or caregivers |
| Unusual injuries based on age and developmental level | Isolation from friends/family; sudden lack of contact from outside friends/family |
| High occurrence of UTIs or injuries to genitalia/rectum | Withdrawal, depression, helplessness, anger, or agitation |
| Unreported old injuries | Unpaid bills, sudden sale or disposal of property/belongings |
| Poor personal hygiene | Poor personal hygiene; presence of rashes, sores, or lice |
Problems
The problems that may be associated with psychiatric emergencies include:
- Risk for Suicide
- Ineffective Coping
- Hopelessness
- Risk of violence against self or others
Treatment
Generally, nurses cannot prevent an individual’s experience of crises. However, nurses can help mitigate the detrimental effects of crisis. To facilitate effective navigation of crises, nurses should:
- Help individuals consider alternate perceptions of the crisis (e.g., growth opportunity)
- Assist the individual in recognizing and utilizing existing support systems
- Cultivate new methods of adaptive coping mechanisms (Videbeck, 2020).
If an individual expresses thoughts of self-harm or harm to another person, this typically results in admission to an acute psychiatric treatment facility. Admission to an acute psychiatric care facility can be on a voluntary or involuntary basis. In the U.S., most states have laws addressing civil commitment or involuntary admission (Videbeck, 2020). Typically, these laws allow detaining for 48-72 hours, until a legal determination can be made as to the individual’s threat of harm to themselves or others (Videbeck, 2020).
Suicide
Individuals verbalizing suicidal thoughts are typically admitted to an inpatient psychiatric treatment facility. Upon admission to an acute care facility, patients and their belongings are searched. Acute care organizations typically have policies that delineate unsafe items (e.g., sharp objects, shoelaces, belts, and lighters). Generally, they are issued a hospital gown or scrubs, and their belongings are stored until they are discharged from the facility. Single-use personal care items are issued on an as-needed basis by the facility. Within the acute care environment, nurses should use suicide safety precautions with individuals verbalizing suicidal thoughts. The goal is to ensure a safe environment for the patient.
Videbeck (2020) guides on implementing suicide safety precautions. Depending on the organization’s policy, these precautions may include:
- Removal of any items that could be used for harm (e.g., sharp objects, belts, shoelaces, metal objects, pens/pencils, clothing with drawstrings)
- One-to-one observation (i.e., in direct sight of staff at all times)
- Other considerations: finger foods for meals, no private rooms
Aggression/Violence
Interventions specific to aggression and violence entail careful consideration of the patient’s legal right to the least restrictive environment to meet their needs (Videbeck, 2020). The least restrictive environment has two main implications.
- If outpatient treatment is sufficient, inpatient treatment is not warranted
- Restraints and seclusion are only used if necessary (Videbeck, 2020).
How can nurses manage aggressive behavior?
Always make sure to follow the institutional policy for the management of aggressive or violent patients. Below is an outline of the steps nurses can use to intervene with an aggressive patient (Videbeck, 2020). When reading over these steps, picture a ladder to remind you that these are progressive interventions and uphold the patient’s right to the least restrictive environment. Meaning, if verbal de-escalation (the bottom rung of the ladder) is sufficient in averting violent behavior there is no need to continue intervention progression, including the use of restraints (the highest rung of the ladder).

- Ensure scene safety, when in doubt do not act alone
- Attempt verbal de-escalation-use a calm, firm voice
- Direct the patient to take a voluntary time-out in a quiet area
- Inform the patient that aggressive behavior is not acceptable
- Offer PRN medications to help the patient return to a calm state (e.g., Lorazepam)
- Provide a “show of force/strength” (i.e., gather 4-6 team members to remain in sight with patient interactions; this may be enough to take control of the situation. If the patient continues to escalate to violent behavior, these staff will help to ensure safety should restraints and/or seclusion become necessary
- Use of restraint and/or seclusion per institutional policy with consideration for the Joint Commission standards
- Debrief: Ask the patient about any triggers and alternatives to avoid future patient violent behavior; hold a debriefing session for all involved staff to discuss elements of the situation that were handled well, needed improvement, and any ideas to enhance defusing (Videbeck, 2020).
Abuse and Neglect
As we have noted in previous psychiatric emergencies, the safety and well-being of all involved is essential and the priority; this is no different in an abuse and/or neglect patient situation. Again, do not act alone. If you are a nurse responding to a situation in the community, enlist the help of local law authorities. Do not attempt to intervene in a situation without help. You cannot predict human behavior and a situation can precipitate into imminent danger in a matter of seconds. Nurses are generally named in the state’s mandatory reporting laws. Meaning, that as nurses we must protect the safety and welfare of certain vulnerable populations (e.g., children, elderly, and dependent adults) by reporting known or suspected abuse/neglect (Carlson, 2022).
There are three main considerations for a nurse’s role in abuse/neglect situations.
- Ensure safety
- Know your state’s mandatory reporting laws
- Make referrals as needed (e.g., social support services)
General Nursing Considerations for a Psychiatric Emergency
Let’s consider a few tenets to consider for psychiatric emergency interventions.
- Safety is the priority. In the event of a safety concern, do not act alone.
- In the acute care environment, follow the institution’s protocols for a psychiatric emergency.
- In the community, call 911 or 988 (the National Suicide and Crisis Lifeline).
- Patients have a legal right to a Least Restrictive environment. See the MODULE 6: LEGAL AND ETHICAL ISSUES module for more on this topic.
- Specific to agitated patients, rapid de-escalation is the primary goal (Heldt, 2021). If possible, verbally de-escalate the situation initially. Implement additional de-escalating strategies (e.g., offer a medication and show of force/strength) prior to using restraints. Remember, restraints are always a last resort. Heldt (2021) indicates restraints are associated with physical and mental harm/psychological trauma. Physical harm may include physical injury, organ damage, and death (Heldt, 2021).
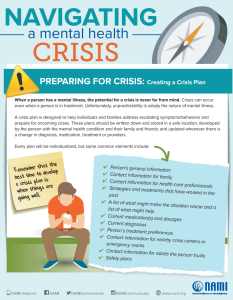
- If possible, help patients create a crisis plan. In fact, this is sound advice for everyone. See “Create a Plan” below.
CREATE A PLAN
Help individuals create a plan of action to help arm them with the tools to navigate a psychiatric emergency. See Nami’s (2022b) resource below. Nurses might also consider recommending individuals complete a psychiatric advance directive. See “Additional Resources” below.
Additional Resources
- Check out the National Resource Center on Psychiatric Advance Directives website
- Consider reading this World Health Organization article (World Health Organization, 2022) for an international perspective on mental health and emergencies
Key Takeaways and Learning Activities
You should have learned the following in this section:
- Crises are individualistic. Meaning, depending on resource availability, what constitutes or results in a crisis for one, may not for another.
- Crises can be classified into three categories (i.e., Maturational, Situational, and Adventitious)
- Individuals expressing suicidal thoughts should always be taken seriously and require immediate action.
- Related to psychiatric emergencies, safety is always the priority. It is often best practice to not act alone. In the acute care setting, nurses must take care to ensure the safety of the patient as well as all within the environment, including healthcare staff and other patients.
- Patients are legally entitled to a least restrictive environment. Verbal de-escalation is the first step in intervention.
- Know your state’s position on mandatory reporting laws. Typically, nurses are state-mandated to report known or suspected abuse/neglect of children, elderly, and dependent adults.
Concept Map Activity
- Create a concept map that depicts the assessment and treatment of Psychiatric Emergencies.
- If needed, see the INTRODUCTION for a concept map tutorial.
Case Study: Psychiatric Emergency
Case Scenario
Natalia, a 24-year-old college student, presents to the emergency room with acute suicidal ideation and self-harm attempts. She denies any medical or psychiatric history. She completed her bachelor’s degree in nursing last month. She works full-time and just received an acceptance letter for a nurse practitioner program. She indicates recently losing her mother in a motor vehicle accident.
Reflective Case Study Questions:
- Assess and describe the immediate nursing interventions for Natalia’s safety.
- Develop a crisis intervention plan for managing Natalia’s suicidal ideation.
- Discuss the ethical considerations in the management of psychiatric emergencies.
- Develop a follow-up plan for Natalia’s ongoing mental health care.
Suicidal ideation entails thinking about killing oneself (Videbeck, 2020).
The patient voluntarily or willing accepts treatment and agrees to hospitalization (Videbeck, 2020).
Individuals, who do not voluntarily or willing accept treatment and hospitalization, may be admitted involuntarily, if they pose a danger to themselves or others (Videbeck, 2020).

