Ethical Considerations
Introduction
The legal and financial aspects inherent in the field of medicine inevitably lead to ethical and professional questions. This chapter is dedicated to exploring these ethical and professional inquiries and lays the groundwork that will be utilized throughout the course. Ethics pertains to the process of deciding how to behave based on a collective assessment of what is morally right and wrong. This can be represented collectively by a profession, a company, an industry, or society as a whole. The determination of what constitutes goodness or rightness is made concerning established ethical standards. While an individual’s personal morals certainly factor into discussions about ethical behavior, it’s important to note that the term “morals” typically implies something distinct from ethics. Morals consist of individual principles linked to one’s conscience that aid in discerning what is right and wrong.
Learning Objectives
-
Identify and analyze various types of ethical issues
-
Compare and distinguish differing ethical and legal issues
-
Interpret the dynamics that give rise to an ethical culture in a healthcare organization
-
Develop a systematic, procedural approach to resolving ethical dilemmas
Ethics and Compliance
Ethics and law are important parts of healthcare. Part of the ethical decision-making process includes the consideration of alternatives. A comprehensive understanding of healthcare laws and how they govern the application of healthcare is needed to make sound ethical decisions. Ethics is often referred to as a person’s personal values or beliefs; furthermore, these beliefs are influenced by an individual’s religion, socioeconomic conditions, geographic location, culture, family, and friends. Healthcare workers must develop a set of beliefs that coincide with their field. For example, a surgical technologist must have a sterile conscience about the sterility of instrumentation and supplies to ensure that patients do not acquire an infection that could be fatal.
To ensure healthcare personnel are making ethical healthcare decisions, a Code of Ethics, similar to standards of care, governs professional organizations. Compliance with these standards is monitored by medical boards, credentialing, licensure, certification, and policies and procedures. Each state has the authority to set standards for credentialing; furthermore, some states offer reciprocity to those credentialed in other states. This recognition allows healthcare providers to practice in different locations without having to repeat the entire credentialing process. Once an individual’s education, training, licensure, and certification have been verified, they are granted privileges. The term privileging means that the board has made sure the provider has the appropriate training and experience to meet the minimum requirements and all authorizations to carry out requested procedures at a specific facility. Credentialing generally refers to primary source credentialing (background check), also known as primary source verification. Lastly, payer enrollment is completed, which is the process by which a medical provider gets entered into insurance plans, networks, Medicare, and Medicaid, so the provider and facility can be paid for services rendered to patients by that provider.
Once privileging is complete, each provider has a determined scope of practice. The scope of practice sets the boundaries determined by the Medical Board and Practice Act. Working outside of the professional scope of practice is not permitted and is considered a violation of the law. It is important to note that if a provider steps outside their scope, malpractice is analyzed using the standards of care they stepped into, not their own.
Healthcare institutions have a fiduciary obligation to maintain moral commitments in the face of challenges posed by economic changes in the delivery of care, which involve organizational integrity. Organizational integrity is essential to the fundamental elements of decision-making and group behavior. This applies not only to societal units in general but also to organizations in particular. What’s even more challenging than the increasing number of healthcare providers engaged in patient care within modern healthcare institutions is the intricate interplay among these individuals and the impact of the organization’s contextual factors on their conduct. It’s often overlooked that many ethical dilemmas in healthcare facilities are beyond the control of individual actors, given that the delivery of patient care is embedded in a complex network of organizational structures, relationships, and processes. Consequently, instead of solely attributing ethical responsibility to individual professionalism, it’s crucial to recognize that the moral dimensions of patient care are significantly shaped by the dynamics of the organization.

Healthcare organizations continuously encounter new sets of ethical issues due to the changes in the delivery and financing of care. The ethics of an organization are deeply rooted in its culture. What do we do when duty conflicts with our interests? Given the complexity and risks associated with the healthcare environment, most health systems have compliance officers who monitor ethics training, corporate policies, and violations of laws. However, ethics and compliance differ. Compliance seeks conformity through mandated rules and regulations. While compliance seeks to avoid litigation or paying fines, ethics seeks to make the right decision for the patient’s health. What do we do when the patient’s welfare conflicts with the financial solvency of the institution? It should be noted that patient care outcomes are largely influenced by the organization’s culture of ethics rather than by individual professionalism. An individual’s behavior informs us that an organization’s corporate culture, structures, and processes are important determinants in achieving organizational integrity (Perry & Thompson, 2017).
Attaining organizational integrity entails a dedicated effort to align the organization’s stated mission and values with decision-making and behaviors at every level of the institution. In essence, an institution must articulate a clear vision and mission, choose a set of guiding values to support its mission, and most importantly, develop a consistent inclination to make choices and take actions that align with these chosen values. In practical terms, organizational ethics centers on the pursuit of organizational integrity.
Developing and maintaining a comprehensive compliance program entails creating and upholding internal policies and procedures designed to prevent any form of illegal, unethical, or improper conduct within the organization. These policies also include establishing standards of conduct and educational and training programs aimed at fostering an environment where individuals are encouraged to report suspected fraud, abuse, waste, or other improprieties without fear of retaliation. Achieving organizational integrity consists of two major components:
a) The culture, rooted in its fundamental values, guides decision-making.
b) The organization’s framework, including its structures and processes, serves as crucial mechanisms for bolstering those core values and ensuring that decisions, actions, and outcomes are in harmony with these foundational principles.
Furthermore, the organization should have a structured approach for addressing alleged violations of rules, regulations, policies, and procedures, as well as internal standards. This involves initiating investigative procedures and overseeing a consistent system for handling any reported violations. Internal communication processes, such as a dedicated compliance or ethics hotline, should be in place to facilitate this reporting mechanism.
In addition to these measures, continuous monitoring is essential across all activities within the healthcare enterprise. This monitoring encompasses various aspects, including research data, institutional review board (IRB) processes, patient records, billing records, marketing efforts, and contractual obligations. The objective is to identify any potential issues related to referrals and payments that could trigger anti-kickback statutes or regulations prohibiting physician self-referral.
Culture
The culture within organizations varies widely, emphasizing a different set of ethical values. There isn’t a universally ideal culture that suits all types of organizations. The prevailing notion is that organizations perform best when their culture aligns with the specific context and strategic goals, meaning they choose values that encourage behaviors crucial for achieving their objectives. For instance, a culture promoting quick decision-making and minimal bureaucracy can boost performance in a competitive mergers and acquisitions advisory firm but might hinder a traditional life insurance company. Similarly, a culture valuing technological excellence benefits a computer manufacturer but wouldn’t suit a symphony orchestra. Finally, organizations prioritizing customer service may prefer a culture emphasizing teamwork, positive customer relations, respect, collaboration, and social responsibility.
While most topics of organizational culture address the values of the employees, it would be amiss not to mention the culture of the community we serve. This includes patients with different ethnicities, social groups, geographical classifications, sexual orientations, religions, etc. The term epoche refers to the suspended personal judgment temporarily. Moreover, a healthcare provider’s personal beliefs about a patient’s cultural components should not hinder their ability to provide care. Oncologist Dr. James Salwitz states,
“Doctors must be without judgment or prejudice and must treat every person without regard to what they believe, what they have done or who they are. Murderer, mother, monster, saint, slumlord, sex offender, nurse, noble or Nazi, the physician is tasked with treating each as human and patient. This creed is not only every doctor’s calling; it is the utopian vision which medicine offers the world… I have learned to see and accept without judgment the human frailties and deviation as part of the constellation of each individual. And to use those traits, even when other forums might judge, to guide and help each patient… The peril is that the shift in tolerance, diversity, and compassion of our society may penetrate so deeply that it will poison even the healers… If blame and hate grow like a disease, it may infect the whole of us… It is our calling not only to care for the sick without judgement but to teach the value of life. The altruistic voice of physicians must remind us of the beauty and potential of all persons, and we must help others see through fear to accept that while we may be different, we are more deeply the same. Any society which holds anyone as “less” by anger, bigotry or hubris has within it a spreading disease. Doctors must heal. They must guide and remind us that in the end, we are all human.”
These cultural beliefs are applicable to any area of care: illness, pregnancy and childbirth, death and dying, etc. While it is our duty to respect all aspects of the patient’s beliefs and wishes, there are times when healthcare must deviate from the patient’s desires to effectively provide care. The most common example is the Jehovah’s Witness blood doctrine. Courts will override parental consent in cases involving life-saving measures for children. Religion also plays a critical role in treatment and healing. Things to consider are dietary restrictions, fasting holidays, medications with animal by-products, herbs/alternative medicines, communication issues, access to care, transportation issues, and gender norms for attending providers. All of these considerations affect the approach to providing care. Physicians, nurses, support staff, and administrators may need to coordinate care with a dietitian, pastoral service, translator, case manager, social worker, hospital general counsel, etc. to fully address the needs of a patient’s cultural preferences. The HELP Model (Connor, 2012) is recommended when working with culturally diverse populations:
Hear what the patient perceives to be the problem.
Encourage the patient and healthcare professional to discuss the similarities and differences.
List treatment options and make recommendations.
Provide a chance to negotiate treatment.
The culture of a healthcare organization may be determined by the type of organization as well. Catholic hospitals have a mission deeply rooted in the healing ministry of Jesus Christ and the Catholic Church. As such, these organizations may omit performing procedures that deviate from the beliefs of Catholicism. They prohibit procedures that are “intrinsically immoral,” including abortion (including ectopic), IVF, contraception (also in the case of rape), physician-assisted suicide, gender reassignment surgery, and direct sterilization. These directives extend to any facilities that involve mergers with a Catholic health facility.
Systems Thinking
Systems thinking in organizational ethics shifts the focus away from individuals as the sole targets for improvement. Instead, it emphasizes understanding interconnectedness, communication, ongoing processes, and root causes of behavior. The goal is to change interactions or redesign the system itself to promote different behaviors. This approach represents a significant departure from the traditional quality assurance approach, which relies on standards and penalties to ensure ethical behavior and primarily centers on individual actions rather than addressing flawed organizational structures and processes. Within a blameless culture, leaders blame processes, not people. This shifts the focus on understanding why something happened, not who is responsible. By striving to identify the root cause of an issue, it creates systems that prevent errors from happening again. This process of depersonalizing mistakes can make a large impact.
While quality assurance is reactive, a systems thinking approach actively seeks to drive change and uphold workplace integrity. It bridges the gap between an organization’s vision/mission and its actual performance, illustrating how the organization’s structures and processes have shaped its current state. Systems thinking also underscores the importance of continuous improvement by demanding constant attention to the structures and processes that influence ethical conduct. This application of systems theory to organizational ethics aligns with the principles of continuous quality improvement and total quality management seen in the healthcare sector, where hospitals aim to enhance the quality of healthcare outcomes.
Developing Organizational Culture
There are several steps to developing a corporate ethical culture. The first is a well-developed mission statement, vision, and guiding values. These define the core values and guiding principles of the organization and set expectations along the path toward achieving its vision. In conjunction, the support of leadership helps develop an ethical infrastructure. Leaders should personally commit to doing the right thing even when no one is watching. According to Perry & Thompson (2017), a good leader is visible and supportive, taking responsibility for making ethical decisions. Other steps include implementing the following:
- Code of Ethics: The organization should establish a clear code of ethics. This code helps to articulate the organization’s values and offers practical guidance on how to apply these values in everyday operations.
- Ethics Forums: Create forums at various levels within the organization where ethical issues can be openly discussed. These forums should include individuals from different hierarchical levels to ensure diverse perspectives are considered.
- Administrative Case Rounds: Develop a formal platform for discussing decisions that impact the ethical aspects of practice and patient care in the organization. This forum should involve both administrative and clinical staff to address issues that overlap their respective areas.
- Appeals Process: Implement a mechanism for principled dissent when individuals have ethical concerns about a practice or policy. Encourage open discussion and resolution rather than punishing those who raise ethical issues.
- Alignment of HR Systems: Ensure that the performance measurement, appraisal, and reward systems within the human resources department are aligned with the organization’s ethical values. This alignment reinforces ethical behavior.
- Ethics Training: Provide ethics training to employees at all levels of the organization. This training should increase awareness of ethical issues, clarify ethical frameworks for decision-making, and enhance ethical decision-making skills, especially in situations involving conflicting values.
- Ethics Officer: Appoint a high-ranking ethics officer to emphasize the organization’s commitment to ethics. This individual would be responsible for integrating ethics throughout the organization, signaling its importance.
- Organizational Ethics Committee: Consider establishing an ethics committee dedicated to addressing the ethical dimensions of organizational issues. This committee would function differently from clinical ethics committees and provide a space for ethical reflection on various organizational matters (Perry & Thompson, 2017).
Monitoring and Evaluating
Monitoring and evaluating ethical performance within healthcare organizations involves various approaches, such as conducting patient and family satisfaction surveys as well as staff satisfaction surveys. Additionally, an ethics climate survey can assess whether the organization aligns with its ethical standards and values. Information systems should provide timely reports on key indicators, including morbidity and mortality statistics, infection rates, incident reports, sentinel events, and patient complaints. Evaluating service performance in terms of specific outcomes, such as pain relief for patients following hip replacements, is also essential. Furthermore, gathering insights through focus groups and interviews can shed light on various ethical situations encountered by different members of the organization, some of which may not be brought to the attention of the clinical ethics committee (Perry & Thompson, 2017).
The increasing emphasis on organizational culture and integrity management in healthcare mirrors trends in the business world over the past few decades. The recognition of the importance of integrity in the workplace grew in response to corporate misconduct and ethical lapses in various industries. These issues were often the result of a failure to integrate integrity into an organization’s culture, structures, and processes. In healthcare, administrators face challenges such as limited financial resources, reduced staffing, intense competition, and the demand for high-quality care. Understanding and addressing the organization’s culture and ethics are essential for effectively managing these challenges. Recognizing the underlying forces can help administrators understand employee behavior, identify necessary organizational changes, and improve overall organizational efficiency. While many may view ethical behavior and legal compliance as common sense, the complexity of organizational relationships necessitates proactive management of the ethical climate to achieve organizational integrity (Perry & Thompson, 2017).
Ethical tendencies of a leader contribute greatly to the outcomes of morale within the organization. Leaders going beyond the typical “boss” role inspire employees and help establish higher morale and better job attitudes and productivity. Employee morale has a direct impact on the ethical tendencies of individuals within an organization. When employees are motivated, satisfied, and have positive morale, they are more likely to exhibit ethical behavior in the workplace. High morale can contribute to a culture of ethics in the workplace. Unfortunately, while the jester of an appreciation with a pizza party may be well intended, it is condescending to support staff when other, more pressing issues need to be addressed. These attempts do little to boost employee morale. A more comprehensive approach is needed, including addressing burnout, clinician wellness councils, mental health programs, cost-of-living/hazard pay, bonuses, recharge rooms, peer support, employee recognition programs, flex work schedules, and remote work when applicable (Gooch, 2023). Organizations lose valuable resources when they focus more on staff recruitment issues than on the retention of current employees.
Mandatory Reporting
Mandatory reporting is a legal requirement that obligates individuals or entities to report certain specific information or incidents to relevant authorities or agencies. The purpose of mandatory reporting is typically to protect public safety, ensure compliance with laws and regulations, and facilitate the detection and prevention of specific issues or abuses. Vulnerable populations of often at greater risk of abuse and deserve special attention. Laws requiring healthcare personnel to report signs of abuse are called mandatory reporting laws (Stanford, & Connor, 2020). Mandatory reporting can cover a wide range of areas, including:
- Child Abuse and Neglect: In many jurisdictions, professionals such as teachers, healthcare workers, and social workers are mandated reporters who must report suspected cases of child abuse or neglect to child protective services.
- Elder Abuse: Similar to child abuse, certain professionals may be required to report suspected elder abuse or neglect.
- Healthcare: Healthcare providers often have mandatory reporting requirements for certain diseases, injuries, or adverse events to public health agencies. This can include notifiable diseases, medical errors, and adverse drug reactions.
- Financial Institutions: Banks and financial institutions may have mandatory reporting requirements for suspicious financial transactions to combat money laundering and fraud.
- Workplace Safety: Employers may be required to report workplace accidents or injuries to occupational safety and health authorities.
- Educational Institutions: Some educational institutions have mandatory reporting requirements for incidents like bullying, harassment, or threats of violence.
- Animal Cruelty: In some places, individuals are required to report suspected animal cruelty or abuse.
- Ethical Violations: In certain professions, such as law and accounting, there may be mandatory reporting of ethical violations by members of those professions to their respective regulatory bodies.
- Domestic Violence: Healthcare providers and others may have mandatory reporting requirements for suspected cases of domestic violence.
Failure to comply with mandatory reporting requirements can lead to legal consequences, including fines or penalties. The specific reporting requirements and who is obligated to report can vary widely depending on the jurisdiction and the nature of the issue being reported. The aim of mandatory reporting is to ensure that potential problems or dangers are identified and addressed promptly in the interest of public welfare and safety.
Difference Between Ethics and Compliance
Ethics and compliance are related concepts in the context of organizational behavior, but they have distinct meanings and purposes. Ethics pertains to the moral principles and values that guide behavior based on what is considered right or wrong, while compliance is about conforming to established rules and regulations to avoid legal consequences and maintain organizational integrity. While both ethics and compliance are essential in organizations, they serve slightly different purposes, with ethics encompassing broader moral considerations and compliance focusing on legal and regulatory requirements. Two prevailing approaches to regulating employee behavior within organizations are the compliance-based and integrity-based models. These two models represent distinct philosophies for managing employee behavior. The compliance-based model relies on external regulation and enforcement, while the integrity-based model focuses on internal self-governance and the promotion of shared ethical values to guide employees in their actions (Perry & Thompson, 2017).
Compliance-based model: This model relies on external regulation and the use of threats and punishments to influence employee behavior. It primarily views employee conduct through a legal and regulatory lens, emphasizing the need to deter illegal or unethical actions and incentivize behavior in line with organizational values. Essentially, it operates on the premise of “comply or face consequences.”
Integrity-based model: In contrast, the integrity-based model takes a different approach to employee management. It emphasizes self-governance, the cultivation of shared values, and the recognition of employees’ ethical aspirations as motivational factors for adhering to rules and standards. This approach aims to instill a sense of employee accountability rooted in a commitment to the organization’s mission. Rather than just teaching employees to follow laws and rules, it seeks to integrate ethics into their decision-making processes and inspire them to embody the company’s ethical ideals.
Both compliance and integrity approaches involve elements like organizational codes of conduct, legal training, and penalties for misconduct. However, the integrity strategy has been proven to encourage responsible employee behavior and a strong ethical identity rooted in the organization’s values. When employees perceive that an organization follows an integrity-based approach, it leads to benefits such as increased commitment to the organization’s mission and a stronger sense of trust in the organization’s support. These positive outcomes are not as prominent in organizations that primarily emphasize employee compliance with rules and regulations. Additionally, employee behavior can be influenced by their perception of the organization’s cultural objectives, whether compliance-oriented or integrity-focused.
Creating an organizational climate of integrity, characterized by self-governance and shared values among employees, is particularly challenging in the complex healthcare delivery system. However, it is crucial for the success of healthcare providers. Healthcare organizations, given their responsibility for the well-being of patients, must strive to establish harmonious work environments where all healthcare personnel can thrive in serving patients. Trust is also a crucial component of building a culture of integrity, and healthcare organizations dedicated to patient care and public health should set an example in fostering cultures of trust and integrity. Emphasizing integrity over mere compliance can lead to more responsible and ethical employee behavior, but creating such a culture in healthcare settings is complex yet essential for the success of healthcare providers and the well-being of patients.
Ethics in Medicine
The relationship between physician and patient is infused with deep trust, intimacy, and vulnerability. Often, exams require a patient to disrobe and answer personal questions. These encounters can be frequently marked by fear, discomfort, and uncertainty regarding the potential life-and-death consequences of decisions made; therefore, authoritarian figures in healthcare must be guided by ethical principles. Regardless of their socioeconomic status or level of education, patients must ultimately trust their healthcare providers with their well-being. There is said to be a gross disparity in the bargaining power of the customer in healthcare (Perry & Thompson, 2017). Financial incentives for providers can clash with patient care, tipping the scales between profit and well-being. In this sense, ethics boil down to daily choices, and in medicine, those choices carry weighty consequences.
When health policy decisions involve making choices between conflicting values and distributing advantages and burdens, ethical reflection becomes indispensable. Furthermore, healthcare is fundamentally a compassionate endeavor, rooted in the notion of providing care rather than being solely profit-driven as seen in other businesses. Given its unique nature, individuals in the healthcare sector, particularly those directly involved in patient care but also those in administrative roles should prioritize ethics. This is essential both as a professional safeguard against the influence of competing economic interests driven by external investors, which could compromise the healthcare profession’s core commitment to patient well-being and as a practical strategy for protecting healthcare providers from medical malpractice liability claims (Perry & Thompson, 2017).
Guidelines for maintaining a professional physician-patient relationship include the following:
- Build trust
- Provide privacy (when dressing and undressing)
- Use appropriate language
- Another healthcare professional should be present during an intimate examination
- Listen to the patient without judgment
- Do not overstep personal boundaries
- Avoid all sexual contact, including flirting
- Do not visit a patient outside of the healthcare setting
- Never make promises to a patient
Resolving Ethical Dilemmas
Our ability to recognize ethical dilemmas is compromised by implicit prejudice, obedience to authority, and time pressures of decision-making. No individual is immune to elements that can compromise our ability to make ethical decisions. The elements are called an unconscious bias. According to UCSF (2023), individual strategies to address unconscious bias include:
- Promoting self-awareness: The Implicit Association Test or other instruments to assess bias are helpful tools to mitigate unconscious bias.
- Understanding the nature of bias is also essential to helping individuals approach their own biases in a more informed and open way.
- Discussions with others (especially those from socially dissimilar groups) can be helpful by promoting conversations in a safe space; furthermore, individuals must be open to alternative perspectives and viewpoints.
- Bias literacy training in the workplace reduces the impact of bias.
What is implicit bias? [YouTube] 2021 by Center for Prevention MN
Healthcare providers and leadership should look beyond the issue of mere legal compliance and finance and pay attention to the dynamics of the situation. Gut instincts can manifest when moral dilemmas are met with ethical blindness. These feelings can manifest as profuse sweating, headaches, or pain in the belly, and such instinctual reactions can often provide very useful signals that moral territory where one’s character is about to be tested may be compromised. When the stakes are high and reputations, stock prices, and people’s livelihoods hang in the balance, emotional reactions are not as rational as once thought. Mitigation and/or resolution of these ethical dilemmas start by gathering and clarifying relevant facts. A complete process of ethical deliberation will yield a logical solution that should be monitored, and steps should be taken to avoid this type of dilemma in the future.
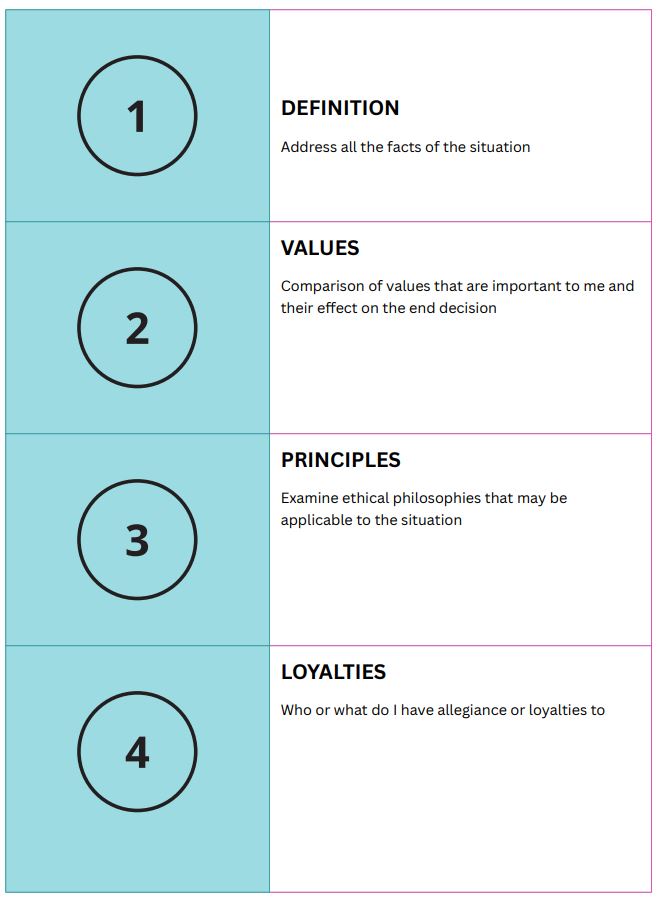
Ethical decision-making, as described by the Potter Box (Hagen, 2017), includes the following:
Key Takeaways
- Ethics refers to the guiding standards of conduct expected of the members of a group.
- Ethics is often used as the basis for creating legal standards where the law reflects society’s view of right and wrong.
- An ethical framework will assist an individual in making an ethical decision and should include deciding legality, establishing the problem clearly, determining relevant values, exploring the views of stakeholders, considering the impact on the decision-maker, and reflecting on possible courses of action.
- A culture of ethics begins with a strong commitment from top management.
- Code of Ethics governs organizations, and compliance with these standards is monitored by medical boards, credentialing, licensure, certification, and policies and procedures.
- Healthcare institutions have a fiduciary obligation to maintain moral commitments in the face of challenges posed by economic changes in the delivery of care, which involve organizational integrity.
- Healthcare organizations continuously encounter new sets of ethical issues due to the changes in the delivery and financing of care.
- Achieving organizational integrity consists of two major components: a) The culture, rooted in its fundamental values, guides decision-making. b) The organization’s framework, including its structures and processes, serves as crucial mechanisms for bolstering those core values and ensuring that decisions, actions, and outcomes are in harmony with these foundational principles.
- Organizational culture is the shared values that have been reflected on and articulated by the members of an organization and have been accepted as the normative for culture.
- Systems thinking is a way of making sense of the complexity of the world by looking at it in terms of wholes and relationships rather than by splitting it down into its parts.
- Mandatory reporting is a legal requirement that obligates individuals or entities to report certain specific information or incidents to relevant authorities or agencies.
- The relationship between physician and patient is infused with deep trust, intimacy, and vulnerability.
- Unconscious bias are social stereotypes about certain groups of people that individuals form outside their own conscious awareness. Everyone holds unconscious beliefs about various social and identity groups, and these biases stem from one’s tendency to organize social worlds by categorizing.
References
- Caldwell-Stanford, C. & Connor, V. J. (2020). Applied law and ethics (2nd ed.). Jones and Bartlett Learning.
- Connor, V. (2012). The HELP model.
- Gooch, K. (2023). Beyond the pizza party: How 9 systems are making meaningful efforts to boost provider well-being. Becker’s Hospital Review. https://www.beckershospitalreview.com/workforce/beyond-the-pizza-party-how-9-systems-are-making-meaningful-efforts-to-boost-provider-well-being.html
- Hagen, H. (2017). My Ethical-Reasoning Process: The Potter Box. WordPress. https://hayleyhagen.wordpress.com/2017/01/27/my-ethical-reasoning-process-the-potter-box/
- Perry, J.E. & Thompson, D.B. (2017). Law and ethics in the business of healthcare. West Academic Publishing.
- Salwitz, J.C. (2017). Should doctors’ personal judgments affect their patients? https://www.kevinmd.com/2017/01/doctors-personal-judgments-affect-patients.html
- UCSF Office of Diversity and Outreach. (2023). Unconscious bias training. https://diversity.ucsf.edu/programs-resources/training/unconscious-bias-training#:~:text=Unconscious%20biases%20are%20social%20stereotypes,organize%20social%20worlds%20by%20categorizing.
The significance of ethical behavior is the desire to be seen behaving in an ethical fashion and the recognition that members of the community owe a duty to society are important factors in shaping decisions.
Asks the question how one should act based upon a group-derived definition of right and wrong.
in the context of healthcare credentialing refers to the process by which a healthcare professional's credentials and qualifications obtained in one state or jurisdiction are recognized and accepted in another.
Making sure the provider has the appropriate training and experience to meet the minimum requirements and all authorizations to carry out requested procedures at a specific facility.
describes the services that a qualified health professional is deemed competent to perform, and permitted to undertake – in keeping with the terms of their professional license.
defines the requirements for the practice of medicine within their borders and gives authority to a medical board to enforce the act’s provisions.
the shared values that have been reflected on and articulated by the members of an organization and have been accepted as the normative for culture.
refraining from drawing conclusions or skepticism
is a way of making sense of the complexity of the world by looking at it in terms of wholes and relationships rather than by splitting it down into its parts.
is a workplace environment that fosters transparency, open communication, and a focus on learning from mistakes rather than assigning blame to individuals or teams.
vary from state to state and involves reporting suspected cases of abuse
are social stereotypes about certain groups of people that individuals form outside their own conscious awareness. Everyone holds unconscious beliefs about various social and identity groups, and these biases stem from one's tendency to organize social worlds by categorizing.
is your ability to perceive and understand the things that make you who you are as an individual, including your personality, actions, values, beliefs, emotions, and thoughts.


