Leading for Safety

Introduction
Most people head to work each day with the expectation of returning home in a similar state of health as when they left. Unfortunately, for a distressingly large number of workers, this expectation does not hold true. Incidents in the workplace persist, and consequences can vary from minor property damage to tragic fatalities. In certain instances, the connection between an injury and a specific workplace factor is immediately evident, such as a roofer fracturing a leg after falling off a ladder, a data entry clerk experiencing arm strain due to repetitive motions, or a nurse sustaining a needle stick injury. However, in other scenarios, establishing a direct link between an injury or illness and the workplace is not immediately apparent. Examples include individuals working in a bar who develop noise-induced hearing loss, custodians who develop dermatitis, or firefighters who develop leukemia after retirement. In these cases, factors like the time elapsed between exposure to workplace hazards or engagement in other activities can complicate the process of linking a workplace factor to an illness (Graham & Rowley, 2017).
Learning Objectives
- Explain How to Create a Culture of Safety in the Workplace
- Identifying Potential Signs of Workplace Violence and Harassment
- Define and Identify Personal Protective Equipment
- Describe the Different Types and How to Identify Hazards in the Workplace
Occupational Safety
According to the U.S. Bureau of Labor Statistics, the United States has more than 3 million incidents of occupational injuries and illnesses reported annually (2021). An injury refers to a sudden and often traumatic wound or physical condition of the body resulting from external forces, which can include stress or strain. Typically, injuries are linked to a specific event, incident, or a sequence of events or incidents that transpire within a single workday or shift. An occupational injury, specifically, is a physical harm that stems from an accident occurring within the workplace. Additionally, occupational illness results in 25 percent of employees taking time off from work to recover or receive treatment.
The roles of occupational safety and health experts have evolved beyond their traditional functions, which included tasks like carrying out safety inspections, providing training, probing into accidents, and pinpointing hazardous behaviors and situations. Nowadays, safety professionals have a broader scope of responsibilities that extend throughout an organization. They actively contribute to fostering innovations in occupational safety and health that can elevate the overall performance of the organization. They collaborate with individuals across all levels within the organization, as well as with government agencies, regulatory bodies, and business associations, to formulate comprehensive occupational safety and health plans and initiatives. This directly affects productivity. Even worse, it is estimated that between 4,000-5,000 people die each year from work-related injuries or illnesses (Graham & Rowley, 2017).
Culture of Safety
A workplace safety culture pertains to the shared attitudes, values, and conduct within an organization that places a paramount emphasis on the welfare and security of its employees. This culture serves as a critical foundation for upholding a secure working environment. According to the Society for Human Resource Management (SHRM) (2008), safety cultures can assume diverse forms, often categorized into four primary types:
- Forced culture- uses bribes and threats to motivate employees
- Protective culture- implements safety programs for employees (policies and procedures)
- Involved culture- characterized by safety training sessions for employees and monitoring performance
- Integral culture- characterized by safety training sessions and safety officers that have budgets and authority
Just Culture promotes reporting mistakes without punitive retaliation to efforts to address and prevent future occurrences. This concept is closely tied to patient safety and recognizing errors or near-misses. It focuses on the processes in place that led to the incident and how to improve those processes, rather than placing blame on those that reported the incident.
Leadership plays an integral role in shaping and promoting a safety-oriented culture. Leaders must lead by example, accord priority to safety, and effectively communicate its significance to the workforce. A robust safety culture is distinguished by its sustained endeavors to elevate safety standards and protocols. This entails ongoing training, the identification of potential hazards, and the establishment of feedback mechanisms. Engaging employees in safety initiatives cultivates a sense of ownership and unwavering dedication to safety concerns. Encouraging the reporting of safety issues without fear of reprisals holds paramount importance.
Safety in terms of healthcare extends not only to the patients but also to the medical professionals and support staff. Whether it be a needle stick, medication errors, or physical assaults, the goal of workplace safety is to create a safe environment for all who enter the facility. It is important to acknowledge that any error resulting in harm or death of a patient is also devastating to the clinicians involved and has been known to lead to self-harm, depression, isolation, and even suicide. Considering the high stakes associated with the impact of enhancing workforce and patient safety, healthcare leadership should prioritize improving quality and safety through its core values.
Safety Culture in Healthcare [YouTube] 2014 by DNV
Workplace Violence and Harassment
Within the healthcare sector, workplace violence (WPV) is acknowledged as a potential danger. WPV encompasses actions or expressions of physical aggression, harassment, bullying, coercion, or any other form of menacing and disruptive conduct that takes place in the workplace. This issue can impact various stakeholders, including employees, patients, customers, and visitors. WPV encompasses a wide spectrum of behaviors, ranging from verbal threats and abuse to physical assaults and, in the most extreme cases, even lethal acts (OSHA, 2012).
People susceptible to workplace violence include individuals engaged in tasks like handling money transactions with the public and interacting with unpredictable or emotionally unstable individuals. Those who operate in solitary or secluded settings may also be more vulnerable to potential violence. Occupations involving the provision of services, caregiving, or work in establishments where alcohol is served could heighten the likelihood of encountering violence. Moreover, variables such as the time of day and the workplace’s location, such as working late at night or in areas characterized by elevated crime rates, should also be taken into account when addressing workplace violence concerns. Among the high-risk groups are employees engaged in cash transactions with the public, delivery personnel, healthcare providers, public service workers, customer service representatives, law enforcement officers, and individuals who work alone. According to the Bureau of Labor Statistics Census of Fatal Occupational Injuries (CFOI), in 2019, there were 761 cases of intentional injury by another person that led to fatalities in the U.S. Women made up 8.6 percent of all workplace fatalities but represented 14.5 percent of intentional injuries by a
person in 2021.
Preventing Workplace Violence
The best prevention is identifying and addressing potential problems early. Workers may exhibit sudden changes of typical behavior, deteriorating job performance, poor relationships with coworkers and patients, refusal to accept criticism or comply with rules, outbursts of rage, odd behavior and isolation, avoidance of eye contact, and/or others who do not want to work with them. Signs of escalating aggression could include pacing, rapid breathing, and/or aggressive posturing. They may begin to speak faster, more loudly, or use a threatening tone. According to the safety video below, de-escalating tense situations in a non-violent manner can be approached by:
- Do not confront an angry person
- Do not get into a power struggle
- Do not roll your eyes, interrupt, or show frustration
- Speak slowly and calmly
- Ask how you can help
- Use their name, if applicable
- Provide options to resolve the situation
- Use terms like “we” and “us“
- Don’t make promises that you can’t keep
- Have witnesses when comforting the angry person
- If necessary, put space between you and the aggressor
Workplace Violence Training for Healthcare Workers [YouTube] 2017 by SafetyVideos.com
In 1996, OSHA published guidelines for preventing workplace violence for healthcare and social service workers, recommending that each facility create its own workplace violence prevention program. Additionally, the American Nurses Association’s recommendations for preventing workplace incivility and bullying include the following:
- Setting a “Zero Tolerance” policy
- Encouraging employees to report violent incidents
- Developing a comprehensive violence prevention program (with security measures in place)
Personal Protective Equipment

The workplace can be fraught with various risks. Personal protective equipment (PPE) serves as a means to safeguard against these risks. While PPE does not completely eradicate hazards, it does mitigate the impact on the wearer. Even when PPE is employed correctly, there remains a slight risk of injury, although such injuries are typically less severe than those incurred when PPE is neglected. It is vital to identify both existing and potential hazards associated with a specific task to determine the most suitable protective gear. Personal protective equipment (PPE) comprises attire and/or gear that employees wear or utilize to lower the risk of injury, illness, or disease resulting from workplace tasks or conditions. It’s important to note that PPE should not be the sole reliance for protection against hazards; rather, it should complement other safety measures. OSHA regulations that address PPE for general industry are specified in OSHA 1910 Subpart I—Personal Protective Equipment. In healthcare, the most common types of PPE are hair bonnets/caps, surgical masks, N-95 masks, gowns (reinforced and isolation gowns), gloves, laser goggles or face shields, and shoe coverings.
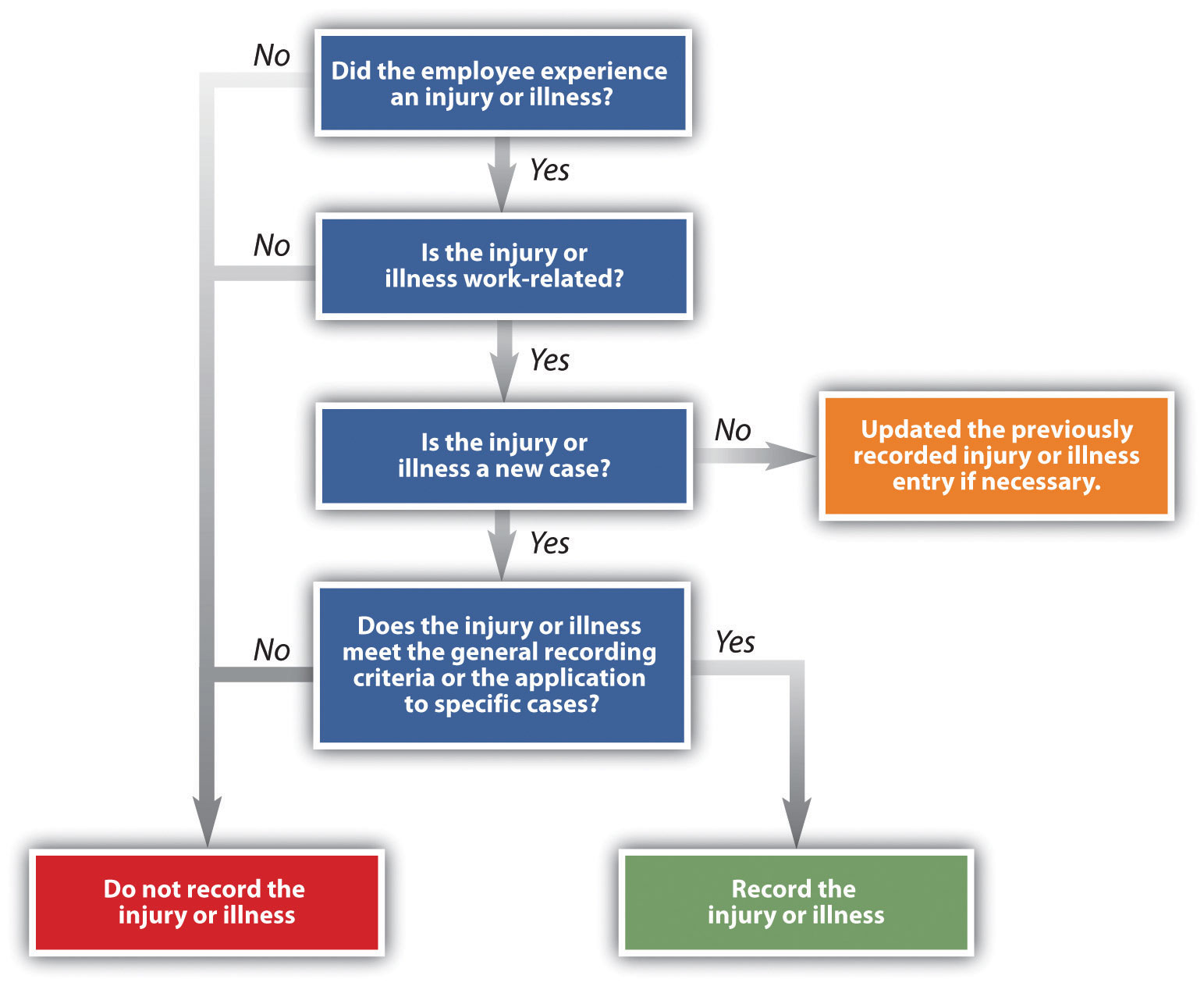
Figure 1. The OSHA Decision Tree for Determining If an Injury or Illness Should be Recorded
Exposure Pathways
According to the Bureau of Labor Statistics Census of Fatal Occupational Injuries (CFOI), exposure to harmful substances or environments led to 798 worker fatalities in 2021, the highest figure since the series began in 2011. OSHA mandates the utilization of personal protective equipment (PPE) to decrease worker exposure to dangers in cases where engineering and administrative measures are impractical or ineffective in reducing exposure to safe levels. Exposure pertains to coming into contact with a substance through ingestion, inhalation, absorption, or injection. Exposure can be categorized as brief (acute exposure), moderate in duration, or extended (chronic exposure). Many hazardous agents have more than one exposure pathway. This term refers to the methods of injury a person may contact a hazard through either absorption, inhalation, or physical contact.
The Shocking Story of the Radium Girls: What the Past? [YouTube] 2021 by Colossal Cranium
1. Absorption
Toxic or hazardous materials can enter the body by permeating the skin, eyes, or mucous membranes. Absorption through the skin can happen without notice to the person being exposed, which is common with chemicals in the workplace. Once the toxic material penetrates the skin, it can enter the bloodstream.
2. Inhalation
Toxic or hazardous materials in the form of gases, fumes, and aerosols can be breathed through the nose and mouth, gaining access to the respiratory system. Inhalation hazards can exist in the air. The concentration of the substance and exposure time will determine the amount of harm. The cycle of air exchange in areas like surgical unions should also be monitored for air quality.
3. Physical Contact
Contact between two people or between a person and an object can lead to injury. Any compromised skin integrity, such as lacerations, punctures, or scrapes, can allow pathogens or hazardous materials to enter the body. Injuries by contusion, burns, or crushing are also categorized as physical contact.
4. Additional Hazards Considered
Each workplace should have current guidelines for potential hazards that a worker may encounter in the workplace and training for appropriate methods for handling these hazards. X-ray radiation, noise, chemical eye hazards, radiant energy, and biological agents should all have policies and guidelines for use and potential exposure. This includes the proper methods of handling and disposing of laboratory chemicals, biohazardous materials, and waste.
Safety Laws
Most safety laws are a result of the Industrial Revolution and lobbying for safety regulations and safe working conditions. Factories were riddled with numerous hazards. Mass production during the war required women and children to work long hours exposed to these hazards. The earliest laws addressed working conditions to prevent injuries. Congress passed the Walsh-Healey Public Contracts Act in 1936, authorizing the Department of Labor to ban federal contracts for work performed under hazardous conditions. The Occupational Safety and Health Act of 1970 was the primary law established in the U.S. to ensure the safest and healthiest working conditions possible for everyone. According to this Act, employers have a legal responsibility to provide safe and healthy working conditions and to comply with occupational safety and health standards. Overseeing federal agencies includes:
The Occupational Safety and Health Review Commission- is an independent federal agency that reviews enforcement priorities, actions, and cases. The National Institute for Occupational Safety and Health (NIOSH)- is a federal agency responsible for conducting research and making recommendations for preventing work-related injury and illness. The Occupational Safety and Health Review Commission (OSHRC)-is an independent federal agency that reviews enforcement priorities, actions, and cases. General inspections and citations for violations are conducted by a compliance safety and health officer (CSHO). Serious violations could result in fines between $1,500 and $7,000 depending on the severity. Willful violations could be fined between $250,000 and $500,000 and/or up to 6 months imprisonment. Repeat violations within a three-year period could be fined up to $70,000.
While there are many agencies that provide oversight for specific industries such as mining, highway safety, pipelines, nuclear energy, and much more, The Food and Drug Administration (FDA) established standards for food, medications, vaccines, tobacco, blood and tissue products, medical devices, cosmetics, and products emitting electromagnetic radiation. Established under Nixon in 1970, the Environmental Protection Agency Environmental Protection Agency (EPA) developed standards to enforce environmental regulations. Environmental regulations are created from environmental acts including the National Environmental Policy Act, the Clean Air Act, the Clean Water Act, the Resource Conservation and Recovery Act, and the Comprehensive Environmental Response, Compensation, and Liability Act.
Additional Employee Protection Laws
The U.S. Department of Labor enforces over 180 federal labor laws (Kurt, 2022). The coverage can vary from unemployment insurance benefits, Social Security benefits, healthcare coverage, and safety laws. According to Kurt (2022), other employee protections include:
- The Fair Labor Standards Act (FLSA) covers various labor standards, including minimum wage and workplace safety regulations.
- Whistleblower protections protect employees from retaliation when they report unsafe conditions or illegal activities in the workplace.
- The Civil Rights Act Title VII of 1964 made it illegal to discriminate based on “race, color, religion, sex, or national origin. In 2020, it added protections for the LGBTQ+ class of workers.
- The Lilly Ledbetter Fair Pay Act of 2009 prohibits wage discrimination against women and minorities.
- Family and Medical Leave Act (FMLA) signed into law in 1993 by President Clinton provides eligible employees up to 12 weeks of unpaid leave per year in the cases of childbirth, adoption, or serious personal or family member illness.
- Thirty-six U.S. states (and the District of Columbia) recognize an implied contract exception to the at-will employment doctrine. Employees cannot be fired except for good cause when a contract is implied. Additionally, employers may be found liable for breach of contract otherwise. However, the employee has the burden of proof (Muhl, 2001).
Workers’ Compensation
Workers' compensation is a government-mandated program that provides benefits to workers who become injured or disabled while performing their job duties (Kagan, 2023). The purpose of worker’s compensation is to ensure that injured employees receive the appropriate medical care and compensation for lost wages if they are injured on the job. Coverage varies from state to state and requires the employee to follow specific reporting guidelines.
It is important to note that some businesses can file for workers’ compensation exemptions for the self-employed, independent contractors, and/or volunteers. Other state exclusions include those with mental health issues (not work-related), injuries from a fight or self-inflected, and injuries received away from work. When an employee is designated as ‘workers’ compensation exempt,’ it signifies that they lack coverage under workers’ compensation insurance. If such an employee sustains a work-related injury or illness, they will not be eligible for benefits aimed at aiding their recovery. Consequently, they, or their employer, will be responsible for bearing the costs associated with medical bills, ongoing healthcare expenses, and treatment outlays. Furthermore, if an exempt employee is unable to work due to a job-related injury or illness, they will not receive compensation for lost wages.
Workplace Wellness
Workplace wellness encompasses initiatives and strategies that encourage and promote positive health behaviors among employees. This can range from conducting health screenings and organizing health education events to implementing fitness programs and offering healthcare benefits, demonstrating various ways in which organizations can cultivate a culture of well-being. This concept has been highly recognized given the global pandemic, economy, and political climate stressors over the last few years. Why is this important to healthcare leaders?
- Healthy workers absorb less healthcare costs
- Healthy workers have fewer absences from work and fewer road accidents
- Healthy, happier workers are easier to retain (Aldana, 2023)
Healthy workers are beneficial to employee morale, organizational culture, and the bottom line. Organizations must commit to investing time and resources into meaningful support endeavors. Wellness programs that focus on the detrimental consequences of smoking, maintaining a healthy weight, addressing depression, managing stress, and alleviating emotional strain due to work-related factors can address the most significant concerns and challenges faced by employees. Creating policies that support healthier living and encompass aspects of physical and mental health, as well as encouraging preventative care are good starting points.
Effective Workplace Wellness
Approaches to improve workplace wellness start with effective onboarding. Provide professional development for continued educational growth and encourage team-building. Gone are the days of 40-hour work weeks being chained to a desk. If feasible, employees prefer flexible work schedules or the ability to work from home occasionally. Some incentives, according to Forbes (2023), to boost employee wellness include:
- Offer competitive salaries and raises
- Create mentorship initiatives
- Remote work
- Flexible scheduling or reduced workdays
- Encourage a work-life balance
- Recognize and reward employees
- Create a culture that employees want
- Provide lifestyle coaching (Mediation/Yoga)
- Teamwork
- Addressing and preventing employee burnout
- Wellness offerings
- Job perks
- Professional development
- Allocate a healthy budget to retention, not just recruitment
- Create a wellness team
- Build employee engagement
Employee Engagement
Employee engagement should be sincere. Often, employees are asked for their opinions or support on an issue, but the decision has already been determined or the consensus of the employees has no impact on the final decision. This can potentially have a more detrimental impact on morale than completely excluding employees altogether from decision-making. Another warning is providing incentives that do not incentivize but rather reduce morale, such as performance or merit-based raises. Too often, employers will down-rank employees to keep these costs from rising. It can be very degrading when an individual worker is not valued for their hard work and dedication. Moreover, having those poor performance reviews affect their potential income could inadvertently cause lower motivation. Good employees who know their value will leave, and should.
Additionally, employees should have transparent knowledge of the organization’s vision or current state. Communication is critical. This could include potential bonuses and raises, open positions, layoffs, furloughs, and changes in policy. Open, transparent communication builds trust. When employees are not happy, there should be avenues to address those complaints without fear of retribution. Open lines of communication should not be punitive; however, they should follow the proper chain of command or be addressed with the union representative.
Conclusion
Mental and physical workplace safety are interconnected. A safe and healthy workplace addresses both the physical and psychological well-being of employees (and patients), leading to improved safety outcomes and overall organizational success. Leadership should focus on providing safe equipment, implementing safety protocols, and maintaining a hazard-free environment to ensure that employees can perform tasks without the risk of injury or harm. They should also create an environment where employees feel supported and free from excessive stress, harassment, or discrimination. Mental safety is crucial for maintaining a healthy work atmosphere and promoting employee engagement and productivity (Breeneman, 2023).
Key Takeaways
- More than 3 million incidents of occupational injuries and illnesses are reported annually.
- Workplace safety culture pertains to the shared attitudes, values, and conduct within an organization that places a paramount emphasis on the welfare and security of its employees.
- High-risk groups are employees engaged in cash transactions with the public, delivery personnel, healthcare providers, public service workers, customer service representatives, law enforcement officers, and individuals who work alone.
- Personal protective equipment (PPE) serves as a means to safeguard against biological, virologic, chemical, and other hazardous risks.
- Exposure pathways include absorption, inhalation, or physical contact.
- Organization policies, OSHA guidelines, and safety laws were created to protect employees from hazards in the workplace.
References
- Aldana, S. (2023). What is workplace wellness? A complete guide for 2023. WellSteps. https://www.wellsteps.com/blog/2022/03/18/workplace-wellness/#:~:text=Workplace%20wellness%20refers%20to%20health,a%20culture%20of%20good%20health.
- Brenneman, K. (2023). Mental health and workplace safety: Is there a connection? Industrial Safety & Hygiene News. https://www.ishn.com/articles/113566-mental-health-and-workplace-safety-is-there-a-connection
- Crail, C. & Watts, R. (2023). 15 Effective Employee Retention Strategies In 2023. Forbes. https://www.forbes.com/advisor/business/employee-retention-strategies/
- Graham, R. E. & Rowley, L. S. (2017). Occupational Safety and Health. American Technical Publishers
- Kagan, J. (2023). Workers’ Compensation: What It Is, How It Works, and Who Pays. Investopedia. https://www.investopedia.com/terms/w/workers-compensation.asp
- Kurt, D. (2022). Laws that Protect Employees. Investopedia. https://www.investopedia.com/articles/personal-finance/120914/8-federal-laws-protect-employees.asp
- Muhl, Charles (January 2001). The employment-at-will doctrine: Three major exceptions. Monthly Labor Review. https://web.archive.org/web/20060322225959/http://www.bls.gov/opub/mlr/2001/01/art1full.pdf
- Smith, J. J. (2008). Four Types of Corporate ‘Safety Cultures’ Detailed. SHRM. https://www.shrm.org/resourcesandtools/hr-topics/risk-management/pages/typesofsafetycultures.aspx
- U.S. Bureau of Labor Statistics. (2021). Census of Fatal Occupational Injuries (CFOI) Summary, 2021. https://www.bls.gov/news.release/cfoi.nr0.htm
- U.S. Department of Health and Human Services (DHHS), National Institute for Occupational Safety and Health (NIOSH) Publication No. 2012-118, (February 2012)
is a learning culture that is constantly improving and oriented toward patient safety.
Personal protective equipment (PPE) is clothing and/or equipment worn or used by an employee to reduce the possibility of injury, illness, or disease caused by work activities or the work environment.
An exposure pathway is the manner in which an individual comes into contact with a hazard.
is a condition or act that may result in personal injury, damage to equipment, or harm to the environment.
is a written document that informs an employer and employees of the regulations that were violated and imposes a time limit to correct the hazards.
is a safety and health professional employed by OSHA who enforces regulations.
is a violation where there is a substantial probability that death or serious physical harm could result.
is a violation that is committed intentionally and knowingly
is a violation that breaches any standard, regulation, rule, or order where, upon reinspection, a substantially similar violation is found.
is an agency under the secretary of the Department of Health and Human Services that is responsible for food, drug, medical devices, and cosmetic safety.
is an agency of the federal government responsible for preventing, controlling, and abating pollution of outdoor air and water due to solid waste, pesticides, radiation, and toxic substances.
any hiring is presumed to be 'at will'; that is, the employer is free to discharge individuals 'for good cause, or bad cause, or no cause at all,' and the employee is equally free to quit, strike, or otherwise cease work.
is a government-mandated program that provides benefits to workers who become injured or disabled while performing their job duties

